Prediabetes has for many years been viewed solely as a precursor to future diabetes; however, recent findings indicate that it also poses a direct risk to the health of the heart. Even when blood sugar values do not reach a level that is traditionally defined as diabetes, they still increase the chance of developing heart disease, heart failure, and dying early. The elevated sugar levels appear to exist for years in many people before developing into T2DM.
Insulin resistance, or metabolic dysfunction, manifests itself in prediabetes and stresses the heart and blood vessels (s), putting patients at significant risk for complications. Each of the main medical organizations uses slightly different blood glucose cutoffs to define prediabetes; all mean the same thing-there is little doubt in the clinical community that the presence of prediabetes should be taken seriously.
There are numerous estimates of the prevalence of prediabetes in many countries. In the U.S., statistics show that more than one in three adults meet the medical criteria for prediabetes, while the U.K. has close to one in five adults with diabetes and/or prediabetes. In China, approximately four in ten adults have been diagnosed with either T2DM or prediabetes. Estimates for prediabetic status worldwide exceed 1 billion individuals.
The usual recommendations for treating prediabetes include losing weight, eating a healthy diet, and increasing exercise. These strategies have been shown to decrease the risk of developing T2DM and improve blood glucose, blood pressure and cholesterol levels; however, these treatments have not provided a definitive target for reducing long-term cardiovascular risk to date, which has made it difficult for physicians to set an effective target for prevention.
Recent data from an international study suggests that achieving blood glucose normalization may be the essential factor in reducing the risk of long-term cardiovascular disease and death. The normalization of blood glucose values is referred to in medical literature as achieving remission.
This means that achieving remission is much more than simply improving the patient’s blood sugar levels. Fasting glucose levels below 100 mg/dL, glucose levels less than 140 mg/dL two hours after taking the standard oral glucose tolerance test (OGTT), and HbA1c levels less than 5.7% are indicators of prediabetes; however, these three criteria must all be present at once. The question is, how important is getting to this level for long-term health benefits?
To investigate this question, researchers re-analyzed two important studies on diabetes prevention: one from the USA and the other from China. Both studies began as lifestyle modification trials and continued for decades.

The leading author of both studies was Dr. Andreas Birkenfeld, an endocrinologist at King’s College London and University Hospital Tübingen. These findings were published in The Lancet Diabetes & Endocrinology.
According to Birkenfeld, “This study provides evidence against one of the primary assumptions of modern-day preventive medicine. While it is clear that modifying lifestyles is beneficial, the existing data do not support the conclusion that this reduces the incidence of and/or mortality from heart disease in patients who have prediabetes. This study demonstrates, however, that the remission of prediabetes results in a significant decrease in the occurrence of fatal cardiac events, heart failure, and all-cause mortality.”
Two studies conducted more than a decade ago provide evidence for the consistency of these results. In the Diabetes Prevention Program Outcomes Study in the USA, people with prediabetes and overweight were studied, and participants were randomized to receive either lifestyle coaching support, metformin, or placebo, and assigned goals surrounding weight loss and physical activity. Assessments for remission were conducted 12 months after the commencement of the study.
The DaQing Diabetes Prevention Outcomes Study in China was launched in 1986. Participants with poor tolerance to glucose were separated into groups on a diet, an exercise regimen, both, and a control group receiving the standard of care. Remission was determined on members of the study in six years. Participating subjects were tracked for more than three decades.
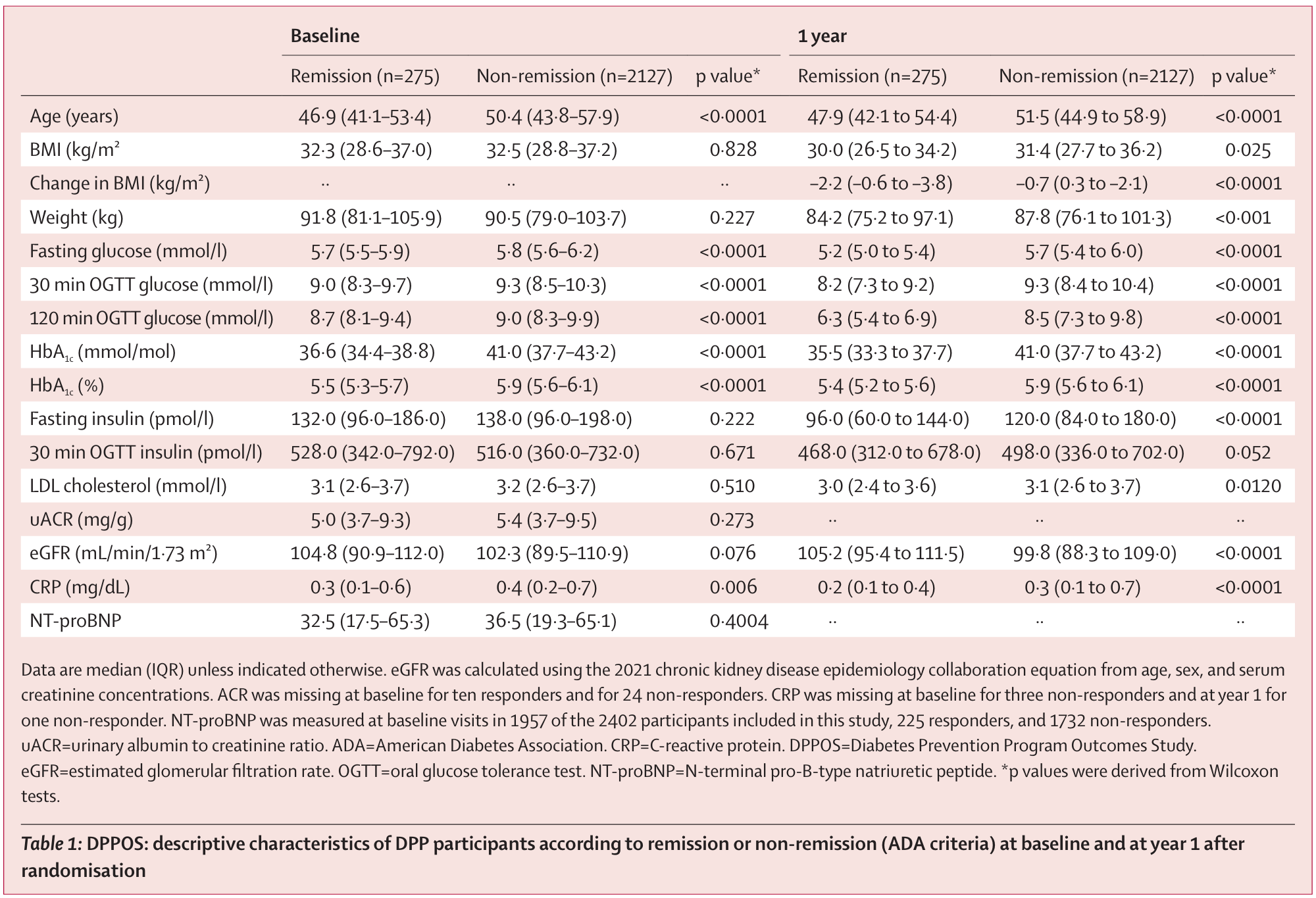
Remission rates were low across both study populations. Approximately 11-13 percent of members of the two groups returned to normal glucose levels. Members returning to normal glucose levels were typically younger and had closer to their baseline glucose levels. Simply losing weight did not fully account for this difference.
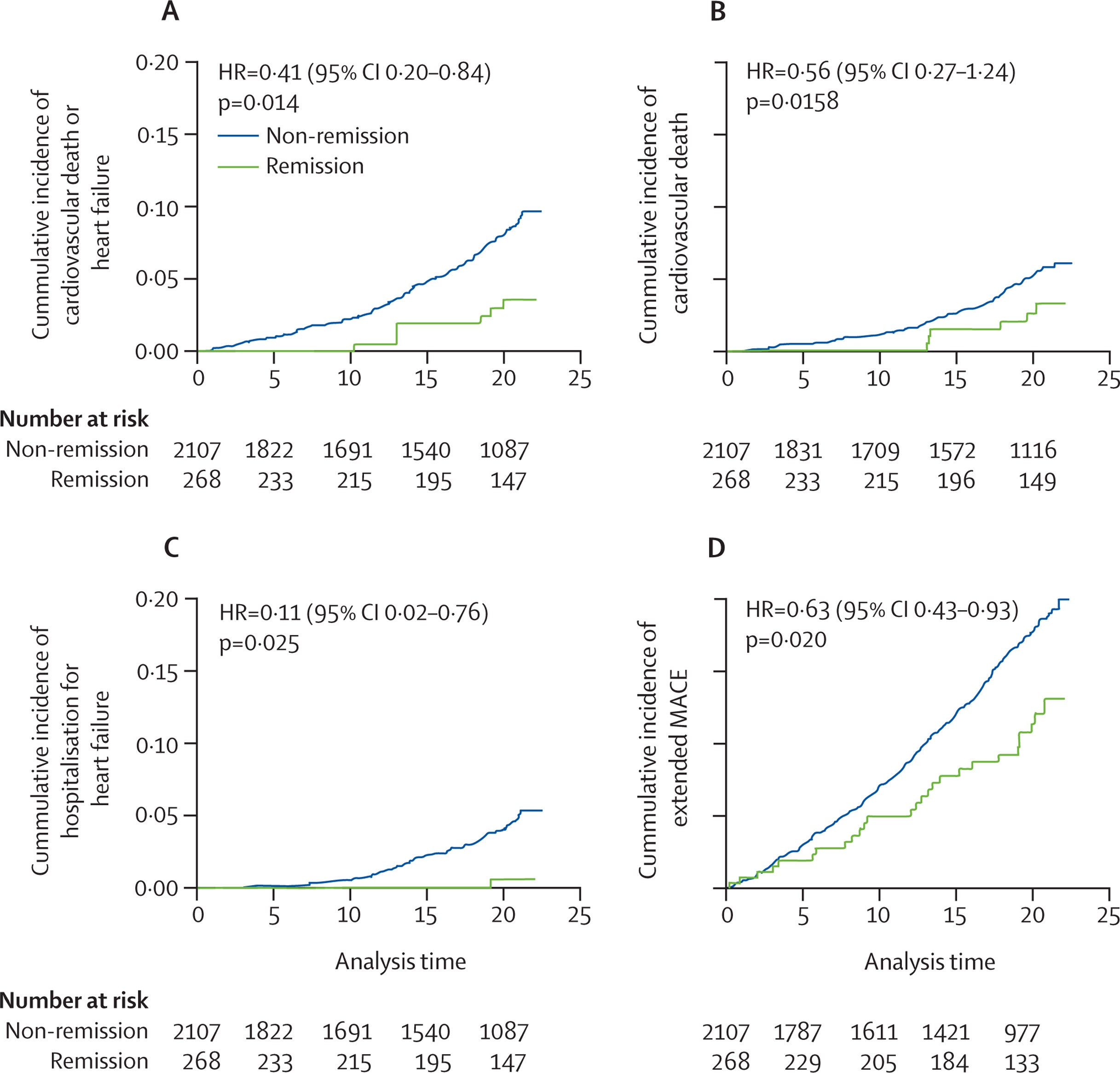
In the U.S. cohort, 34 percent of those participants who achieved remission from diabetes developed type 2 diabetes in progression. In the remaining participants who did not achieve remission from diabetes, 57 percent developed type 2 diabetes. The more impressive finding regarding heart-related events. Rates of vascular death and hospitalization due to heart failure were reduced by over 50 percent.
The findings for the Chinese cohort were almost identical to the U.S. cohort. Participants achieving remission had significantly lower rates of death or hospitalization for heart-related conditions. The participants who achieved remission had far lower rates of overall mortality. The benefits of the lifestyle interventions lasted many years following the cessation of these programs.
The results became more evident when the results from the U.S. and Chinese populations were combined. Participants from both populations demonstrated a 53 percent reduction in the rate of heart disease death or heart failure if they achieved remission from diabetes before final determination. The reduction of death from any cause was over 30 percent in the cases of participants with prediabetes who achieved remission.
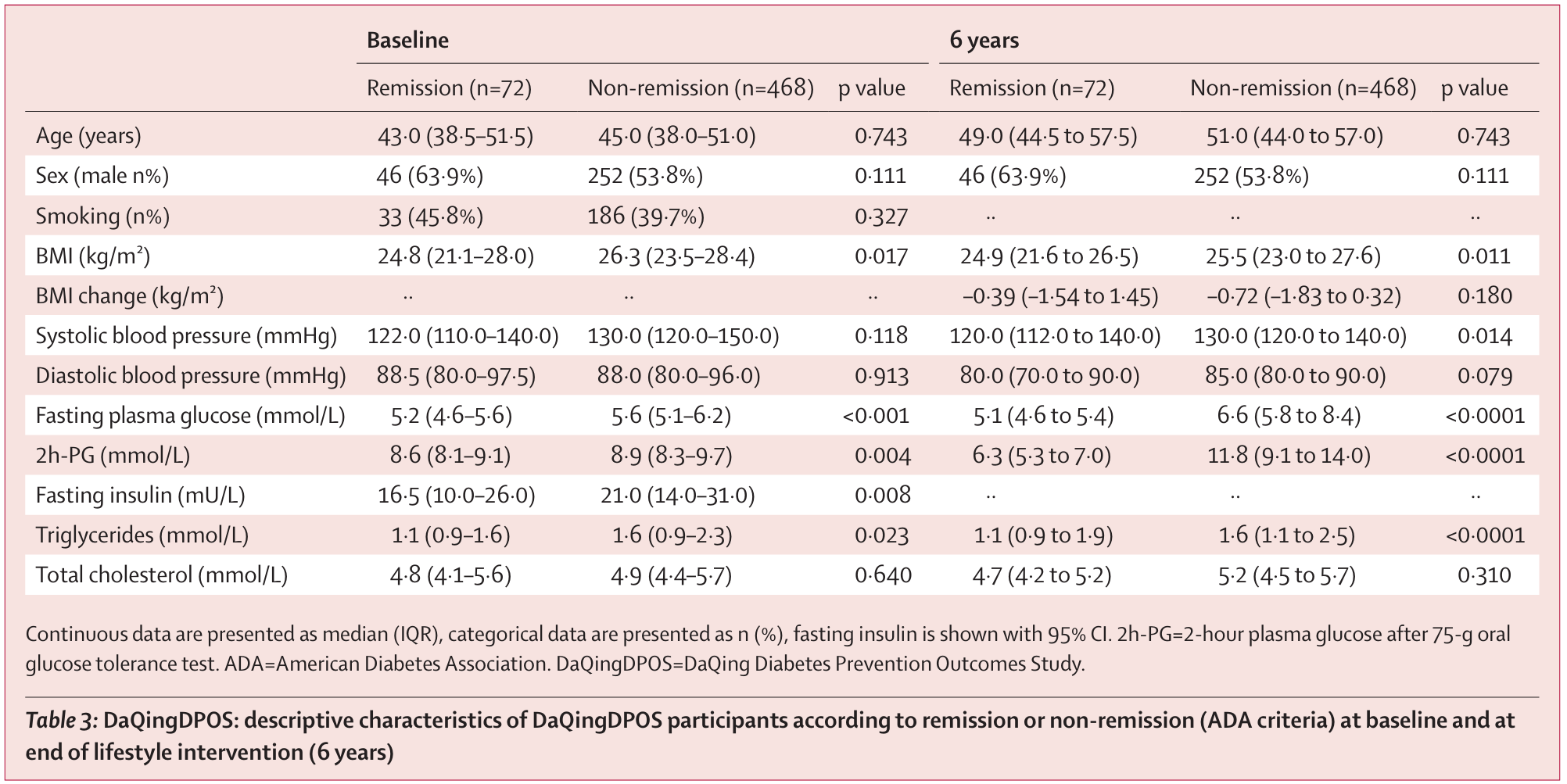
The finding of the heart-related protective effects was the same for participants from both populations, regardless of the country of origin, healthcare system, or ethnicity. Further analysis demonstrated that the heart-related protective benefit was maintained after controlling for age, weight, tobacco use, drugs, and the development of diabetes, after achieving remission.
Researchers considered that there was a simpler marker of the risk of heart disease for clinical use. They found that a fasting glucose level of less than or equal to 97 milligrams may indicate a lower risk of heart disease without the need for additional laboratory tests. This single measurement may provide healthcare professionals with a starting point for future preventive measures against heart disease.
The findings will clarify the previous negative results of lifestyle interventions in regards to heart disease. Exercise and diet have their role, but neither ensures heart protection. Remission provides the opportunity to improve the metabolic changes required for attaining heart protection.
The findings from this study may lead to the revision of disease prevention guidelines.
The three pillars of cardiovascular disease prevention have historically been blood pressure control, lipid reduction, and the cessation of tobacco use. It is possible that remission from prediabetes will become the fourth pillar.
Research findings are available online in The Lancet Diabetes & Endocrinology.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post Lowering blood sugar may cut heart death risk in half — helping over a billion prediabetics worldwide appeared first on The Brighter Side of News.