Alzheimer’s disease, a devastating neurodegenerative disorder, is closely linked to the accumulation of tau protein in the brain. When tau becomes hyperphosphorylated, it forms neurofibrillary tangles (NFTs), disrupting cellular processes and leading to cognitive decline.
Scientists have long known that tau pathology correlates with disease progression, but a groundbreaking study from the University of Cologne sheds new light on the specific role of a particular tau isoform in driving toxicity.
Tau is essential for stabilizing microtubules, the structural components of neurons that facilitate nutrient transport and communication. In the adult human brain, tau exists in six isoforms, each with unique structural properties.
These isoforms are produced through alternative splicing of the MAPT gene, with variations affecting how tau interacts with microtubules. During development, the brain predominantly expresses one form, but by adulthood, it maintains a balance between 3-repeat (3R) and 4-repeat (4R) tau isoforms.
In healthy neurons, tau supports axonal transport and synaptic stability. However, in Alzheimer’s disease, tau undergoes abnormal phosphorylation, detaching from microtubules and aggregating into toxic clumps. This disrupts neuronal function, leading to synaptic loss and, ultimately, cell death.
While amyloid beta (Aβ) plaques have been implicated in Alzheimer’s, they appear to accelerate tau pathology rather than directly cause neurodegeneration. Studies show that reducing tau levels in animal models protects against Aβ-induced toxicity, reinforcing tau’s pivotal role in disease progression.
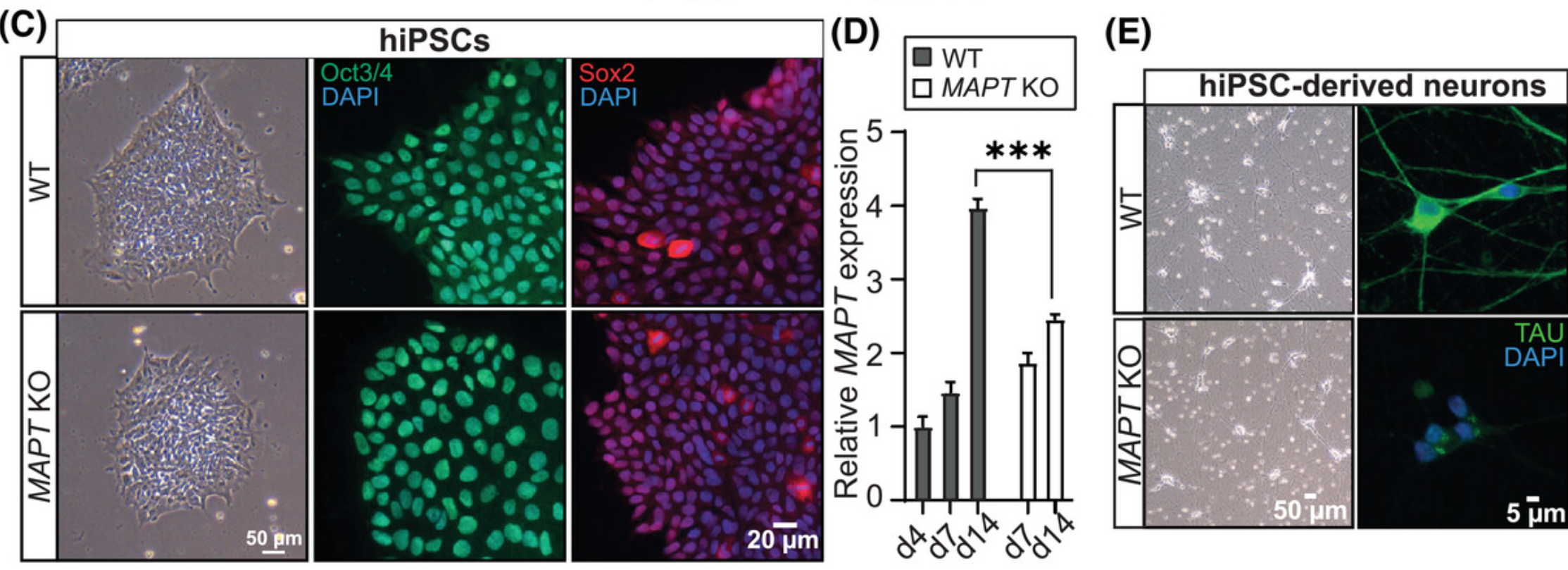
To better understand tau’s role, an international research team led by Dr. Hans Zempel at the University of Cologne used human-induced pluripotent stem cells (iPSCs) to study different tau isoforms.
Their findings, published in Alzheimer’s & Dementia, highlight the 1N4R tau isoform as a key driver of neuronal damage.
Related Stories
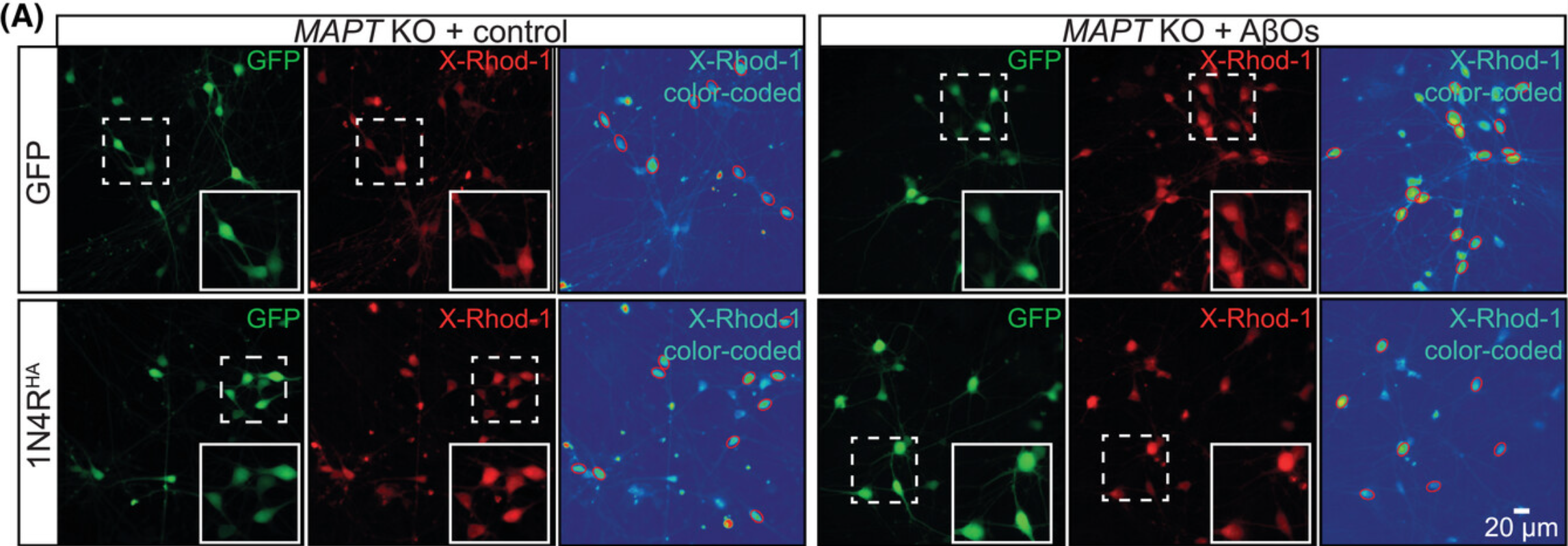
iPSCs, derived from human skin cells and reprogrammed into neurons, provide a powerful tool for studying neurodegenerative diseases in a human context. By using CRISPR/Cas9 gene editing and live-cell imaging, researchers created neurons lacking tau and then reintroduced specific isoforms. This approach allowed them to isolate the effects of each tau variant.
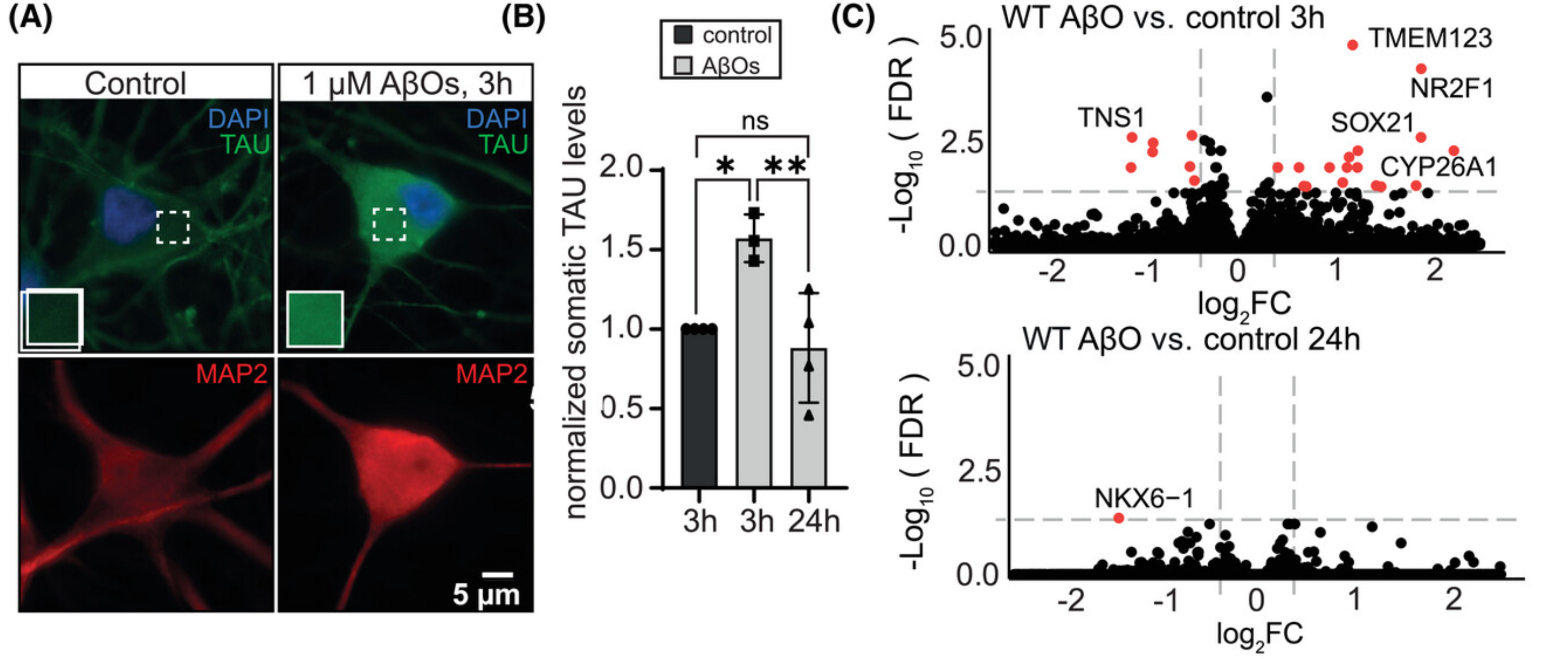
Their results revealed that neurons without tau had impaired neurite growth but were resistant to Aβ-induced toxicity. When 1N4R tau was reintroduced, the neurons regained their vulnerability to toxic Aβ oligomers, confirming its role in disease progression.
Notably, 1N4R tau exhibited higher basal phosphorylation levels in its microtubule-binding region, making it more prone to detachment and aggregation. This suggests that 1N4R tau plays a crucial role in driving tau pathology.
The study’s findings mark a significant step in Alzheimer’s research. According to Dr. Sarah Buchholz, the first author of the study, “This study represents a significant advance in helping us to understand the mechanisms of Alzheimer’s disease. By identifying 1N4R tau as a key protein, we have discovered a potential new target for future treatments.”
Current treatments for Alzheimer’s focus on reducing amyloid plaques, but these approaches have had limited success in slowing cognitive decline. Targeting tau, particularly the 1N4R isoform, could offer a more effective strategy. Since tau pathology appears later in the disease but is more closely linked to cognitive impairment, interventions aimed at preventing tau aggregation might provide better outcomes for patients.
This research also underscores the importance of using human-derived neuronal models in studying neurodegenerative diseases. Traditional rodent models, while valuable, do not naturally develop Alzheimer’s-like tau pathology.
Unlike humans, rodents predominantly express 4R tau, making it difficult to replicate the full spectrum of disease mechanisms. The use of iPSCs bridges this gap, offering a more accurate platform for testing potential therapies.
While this discovery is promising, further studies are needed to translate these findings into clinical applications. Researchers must validate their results in animal models that better reflect human tau expression and develop therapeutics that specifically target 1N4R tau.
The next steps involve screening small molecules or biologics that can prevent 1N4R tau from becoming hyperphosphorylated or aggregating.
The search for Alzheimer’s treatments has been challenging, but this study provides a new direction. Understanding the role of tau isoforms could unlock novel therapeutic strategies, bringing hope to millions affected by this debilitating disease.
Scientists do not yet fully understand what causes Alzheimer’s disease. There likely is not a single cause but rather several factors that can affect each person differently.
In 2010, the costs of treating Alzheimer’s disease were projected to fall between $159 and $215 billion. By 2040, these costs are projected to jump to between $379 and more than $500 billion annually.
Death rates for Alzheimer’s disease are increasing, unlike heart disease and cancer death rates that are on the decline.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post Major new study identifies key protein driving Alzheimer’s disease appeared first on The Brighter Side of News.