Skin cancer is a pervasive global health issue, with melanoma as its deadliest subtype. Responsible for 80% of all skin cancer deaths, melanoma highlights the urgent need for early and accurate detection. Research shows that delays in diagnosis can reduce five-year survival rates by as much as 20%.
However, traditional diagnostic methods, such as the widely used 7-point checklist (7PCL), primarily focus on melanoma. This narrow scope has limited their effectiveness in detecting other types of skin cancers like basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
A groundbreaking study led by researchers from Anglia Ruskin University, the University of Essex, Check4Cancer, and Addenbrooke’s Hospital introduces a revolutionary approach. Their artificial intelligence (AI)-based framework not only expands detection capabilities across all skin cancer types but also significantly outperforms existing methods in sensitivity and specificity. This innovation is expected to redefine how skin cancer is identified, managed, and treated.
Skin cancer diagnosis in the UK follows a two-week pathway system for urgent referrals. This process prioritizes patients with suspicious lesions for specialist evaluation within two weeks. While effective in theory, the system faces significant challenges in practice.
Referrals for skin lesion analysis have surged dramatically, increasing from 159,430 in 2009 to over 506,000 by 2020. Non-urgent cases, such as those involving BCC, often experience waiting times of 18 weeks or longer. Only 80% of patients with non-urgent referrals are seen within this target timeframe.
Complicating matters further, the COVID-19 pandemic disrupted healthcare systems, leading to delays and a substantial diagnostic backlog. An estimated 17% of melanoma cases in Europe were diagnosed at a later stage post-lockdown, underscoring the critical need for faster, more accurate detection tools. Current methods, like the 7PCL and Williams score, have proven inadequate, with sensitivity levels of only 62% and 60%, respectively.
Recognizing these gaps, researchers turned to AI, leveraging its power to analyze vast datasets and identify patterns that traditional methods overlook. The result is a comprehensive framework that utilizes clinical metadata to detect suspicious lesions with unprecedented accuracy.
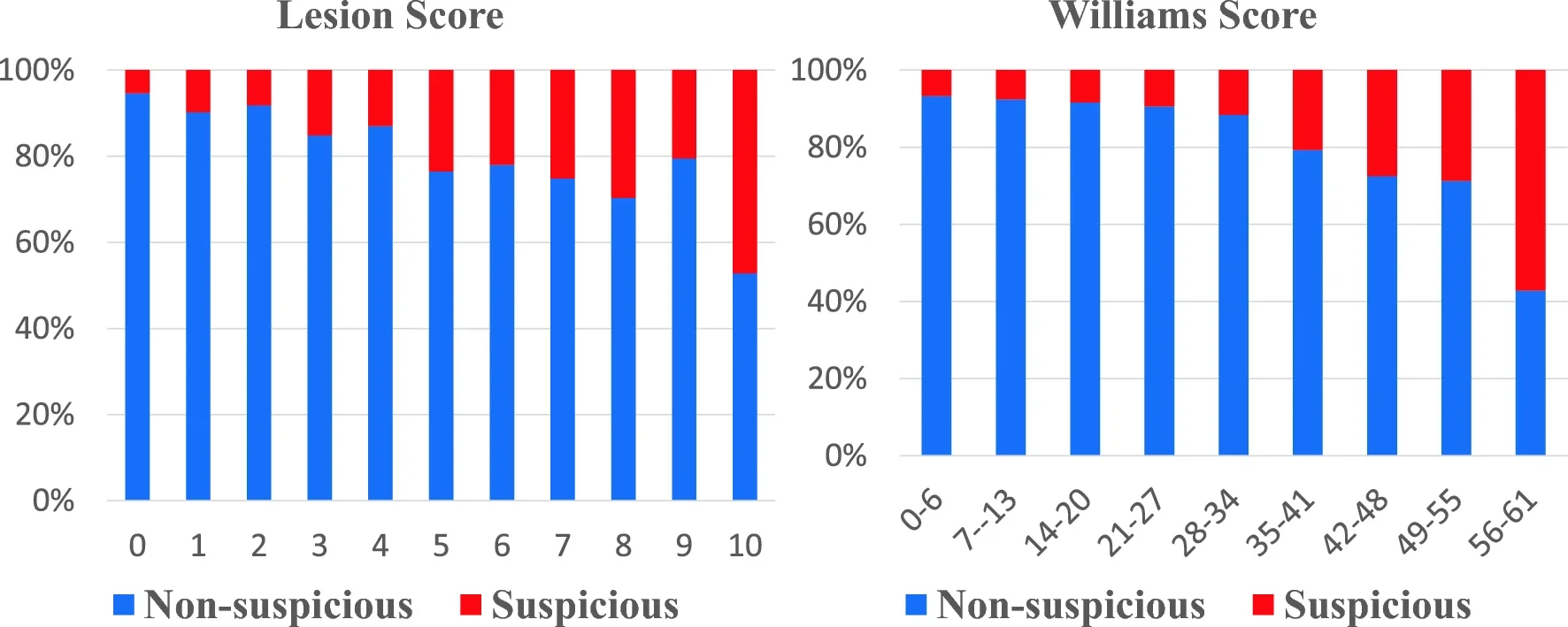
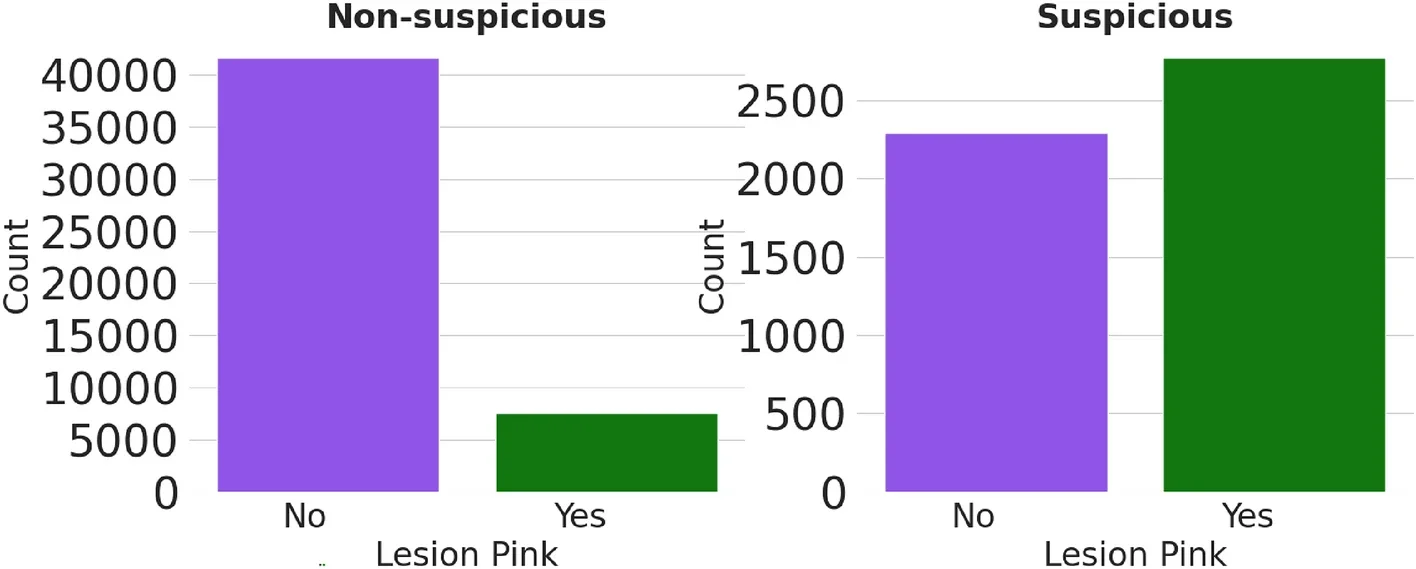
At the heart of this new framework are the C4C risk factors—a set of seven clinical features that predict skin cancer risk across all subtypes. These factors include lesion characteristics such as size, color, shape, and inflammation, as well as patient-specific attributes like natural hair color at age 15 and lesion age. Unlike traditional methods, which focus exclusively on melanoma, the C4C risk factors account for non-pigmented lesions and other forms of skin cancer.
Related Stories
Through machine learning, researchers distilled 22 clinical features into these seven key factors, applying proportional weighting to create the C4C risk score. This score achieved a sensitivity of 69%, significantly outperforming the 7PCL and Williams scores. Professor Gordon Wishart, Chief Medical Officer at Check4Cancer, emphasized the importance of this advancement:
“This study shows the importance of using clinical data in skin lesion classification, which should help improve the detection of skin cancer.”
The researchers’ work involved analyzing metadata from over 53,600 skin lesions collected across the UK. This extensive dataset enabled the development of an AI framework capable of classifying lesions as suspicious or non-suspicious with remarkable precision.
One of the study’s most significant findings is the enhanced performance achieved by combining the C4C risk factors with traditional methods like the 7PCL and Williams score. This fusion resulted in the highest overall sensitivity and specificity, making it the most reliable diagnostic tool to date.
The AI model also demonstrated its potential to reduce unnecessary biopsies and streamline diagnostic timelines. By integrating clinical metadata with image analysis, it offers a scalable solution that can be implemented in teledermatology, particularly beneficial in remote or underserved areas.
Consultant Plastic Surgeon Per Hall highlighted the broader implications of this work:
“Emphasis in the past has been on pigmented lesions and melanoma, but other things grow on the skin that need sorting out, such as basal cell carcinomas and squamous cell carcinomas. This work sifts out lesions that are potentially serious while identifying those whose skin is more prone to developing cancers.”
The introduction of the C4C framework marks a pivotal moment in skin cancer detection. With regulatory approval anticipated by 2025, this AI-driven approach promises to alleviate the burden on healthcare systems while improving patient outcomes.
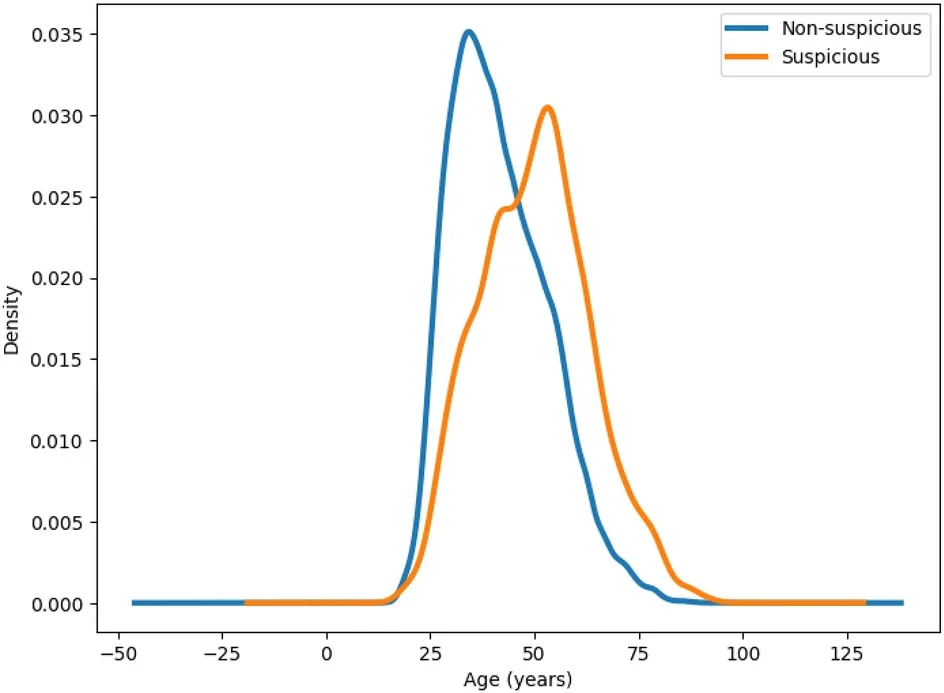
Skin cancer referrals are expected to increase in the coming years due to an aging population and heightened awareness. Innovations like the C4C risk score can help manage this demand by providing accurate, efficient diagnostic tools that prioritize high-risk cases.
Professor Wishart expressed optimism about the future impact of this research:
“Our new AI model could lead to a reduction in the need for patient referrals for biopsies, shorter waiting times for skin cancer diagnosis and treatment, and improved outcomes for patients.”
This study represents a collaboration of experts across multiple institutions, underscoring the value of interdisciplinary research in addressing complex healthcare challenges. Funded in part by a Knowledge Transfer Partnership (KTP) Grant from Innovate UK, the research has been published in Scientific Reports.
The C4C framework is more than a technological achievement; it’s a step toward transforming skin cancer care. By combining clinical expertise with AI’s analytical power, this approach sets a new standard for early detection and comprehensive care.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post New AI system redefines how skin cancer is identified, managed, and treated appeared first on The Brighter Side of News.