For more than a century, Alzheimer’s disease has been framed as irreversible. Once memory and thinking decline, recovery has not been considered possible. That belief shaped nearly all research, which focused on prevention or slowing damage, not repairing it. Now, researchers from University Hospitals, Case Western Reserve University, and the Louis Stokes Cleveland VA Medical Center report evidence that challenges this assumption.
The study, led by Kalyani Chaubey, PhD, from the Pieper Laboratory and published in Cell Reports Medicine, tested whether brains with advanced Alzheimer’s-like damage could recover. Using multiple mouse models and human brain tissue, the team found that restoring balance to a central cellular energy molecule, NAD+, not only prevented disease features but reversed them, even at late stages.
The senior author, Andrew A. Pieper, MD, PhD, directs the Brain Health Medicines Center at the Harrington Discovery Institute at University Hospitals. He also holds faculty appointments at Case Western Reserve University and serves as a clinician-scientist at the Cleveland VA. Together, the team set out to test an idea rarely explored in Alzheimer’s research: recovery.

Nicotinamide adenine dinucleotide, or NAD+, helps cells turn nutrients into energy and repair daily damage. It supports DNA repair, controls inflammation, protects the blood-brain barrier, and keeps nerve cells connected. As you age, NAD+ levels decline throughout the body. In Alzheimer’s, the drop is sharper and more damaging.
“By examining human Alzheimer’s brains and engineered mouse models, our researcher team showed that NAD+ balance was severely disrupted. Cells could no longer meet energy demands or defend themselves against stress. This failure appeared early and worsened as disease progressed,” Chaubey told The Brighter Side of News.
“The team focused on restoring NAD+ homeostasis, meaning healthy balance rather than excessive levels. We used a compound called P7C3-A20, developed in the Pieper lab, which helps cells maintain normal NAD+ under stress. Importantly, it does not push NAD+ above safe levels, unlike some over-the-counter supplements,” he continued.
To model Alzheimer’s, the researchers used two types of mice. One carried human mutations linked to amyloid buildup. The other carried a human mutation in tau, another hallmark of the disease. Both models developed memory loss, inflammation, blood-brain barrier breakdown, nerve damage, and behavioral changes similar to those seen in people.
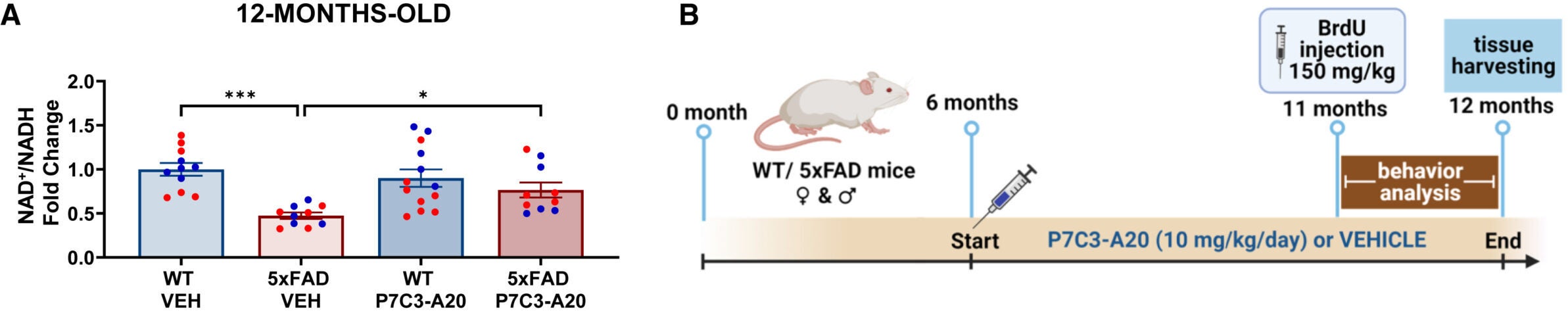
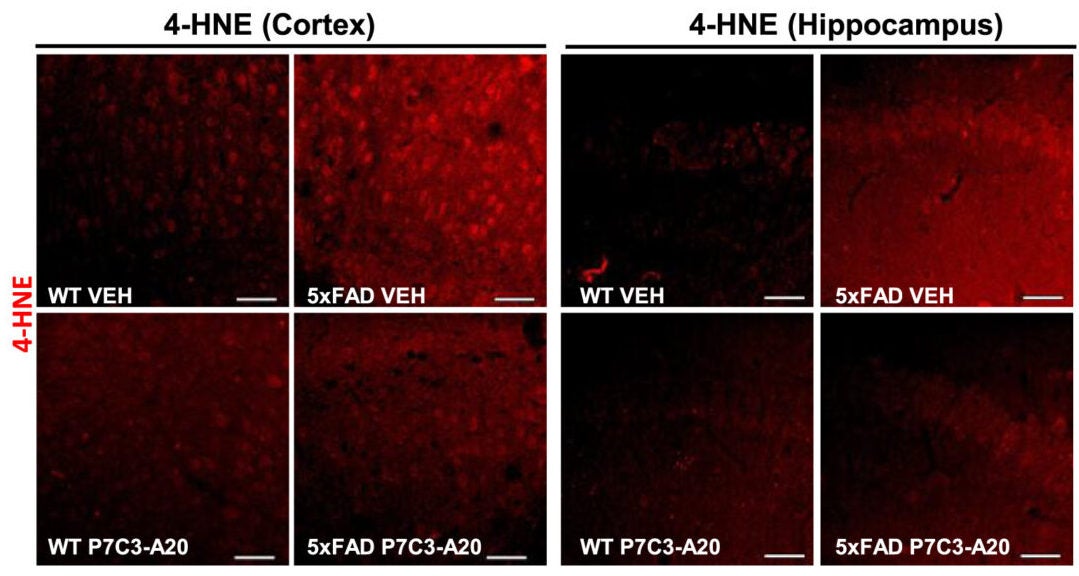
When P7C3-A20 was given before symptoms began, it prevented disease features. More striking was what happened when treatment started later. Mice with advanced disease regained normal NAD+ balance. Brain structure improved. Memory and learning returned to near normal levels.
In maze tests that measure spatial memory, untreated mice struggled. Treated mice performed like healthy controls. In object recognition tests, which measure recall, the same pattern appeared. Even mood-related behaviors normalized after treatment.
“We were very excited and encouraged by our results,” Pieper said. “Restoring the brain’s energy balance achieved pathological and functional recovery in both lines of mice with advanced Alzheimer’s.”
The recovery went beyond behavior. Amyloid plaques were reduced, even though amyloid production itself did not change. That suggests the brain regained its ability to clear toxic proteins. Tau phosphorylation, a damaging chemical change, also declined.
The blood-brain barrier, which normally shields the brain from harmful substances, showed clear repair. Structural gaps closed. Leaky blood proteins stopped entering brain tissue. Cells that support small blood vessels regained coverage.
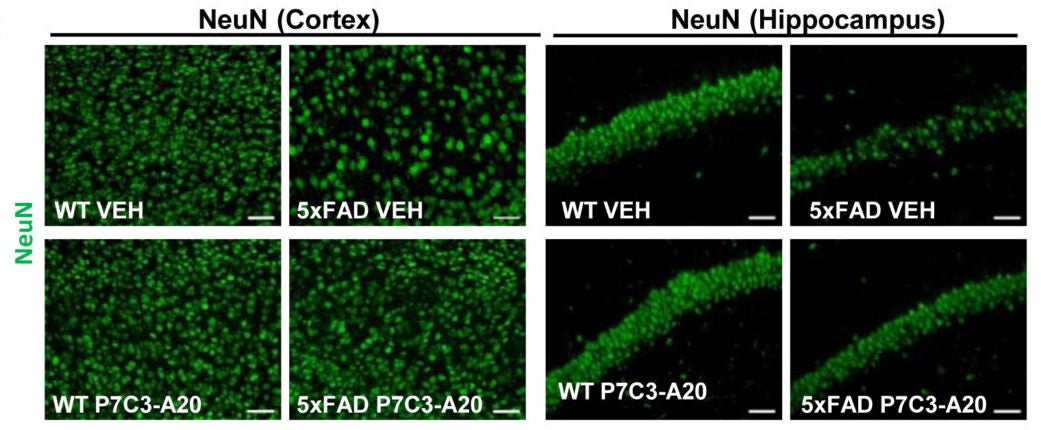
Markers of inflammation and DNA damage dropped. Synaptic function, measured by electrical signaling in the hippocampus, recovered even when treatment began late. Blood levels of phosphorylated tau-217, a clinical Alzheimer’s biomarker, returned to normal, strengthening the case for true disease reversal.
“The key takeaway is a message of hope; the effects of Alzheimer’s disease may not be inevitably permanent,” Pieper said. “The damaged brain can, under some conditions, repair itself and regain function.”
Chaubey added, “Through our study, we demonstrated one drug-based way to accomplish this in animal models, and also identified candidate proteins in the human AD brain that may relate to the ability to reverse AD.”
The team also studied brain tissue from people with Alzheimer’s and from individuals known as nondemented with Alzheimer’s neuropathology, or NDAN. These individuals had heavy plaque buildup but remained cognitively intact.
NDAN brains showed preserved NAD+ balance and healthier protein profiles. In contrast, Alzheimer’s brains showed reduced NAD+ and changes in enzymes that either produce or consume it. These patterns closely matched what was seen in the mouse models.
By mapping thousands of proteins, the researchers identified dozens that shifted in Alzheimer’s and returned to normal with treatment. These proteins are involved in energy production, synaptic health, and cellular cleanup. They may serve as future biomarkers or drug targets.
This work suggests Alzheimer’s may not be a one-way path. If brain energy balance can be restored, recovery may be possible, even after symptoms appear. For patients and families, this reframes the disease from a permanent loss to a potentially reversible state under the right conditions.
For researchers, the findings open new directions. Instead of only blocking amyloid or tau buildup, therapies could focus on strengthening the brain’s own repair systems. Carefully designed human trials will be needed to see if these results translate beyond animal models.
Clinically, the study also raises caution about unsupervised NAD+ supplementation. The approach tested here restores balance without pushing levels too high, an important safety distinction. If confirmed in people, therapies aimed at NAD+ homeostasis could influence treatment strategies for Alzheimer’s and other age-related brain diseases.
Research findings are available online in the journal Cell Reports Medicine.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post New study model shows Alzheimer’s disease can be reversed — not just prevented appeared first on The Brighter Side of News.