The human immune system is a complex network of cells and signals that guards against disease, yet in the case of cancer, it often struggles to mount an effective response.
Recent research, published in the journal, Nature, has unveiled a novel immune cell type, the stem-like CD4 T cell, that could be the key to improving cancer immunotherapies. This discovery sheds light on how these cells can drive robust anti-tumor responses while remaining largely inactive in many patients.
CD4 T cells have long been recognized as essential players in the immune response, particularly in cancer. Their ability to enhance immunotherapy, adoptive T cell therapies, and vaccination strategies has been well-documented.
The differentiation of CD4 T cells into T helper 1 (TH1) or T follicular helper (TFH) subsets is often critical for controlling tumors, while their transformation into regulatory T cells (Tregs) or dysfunctional states is linked to disease progression.
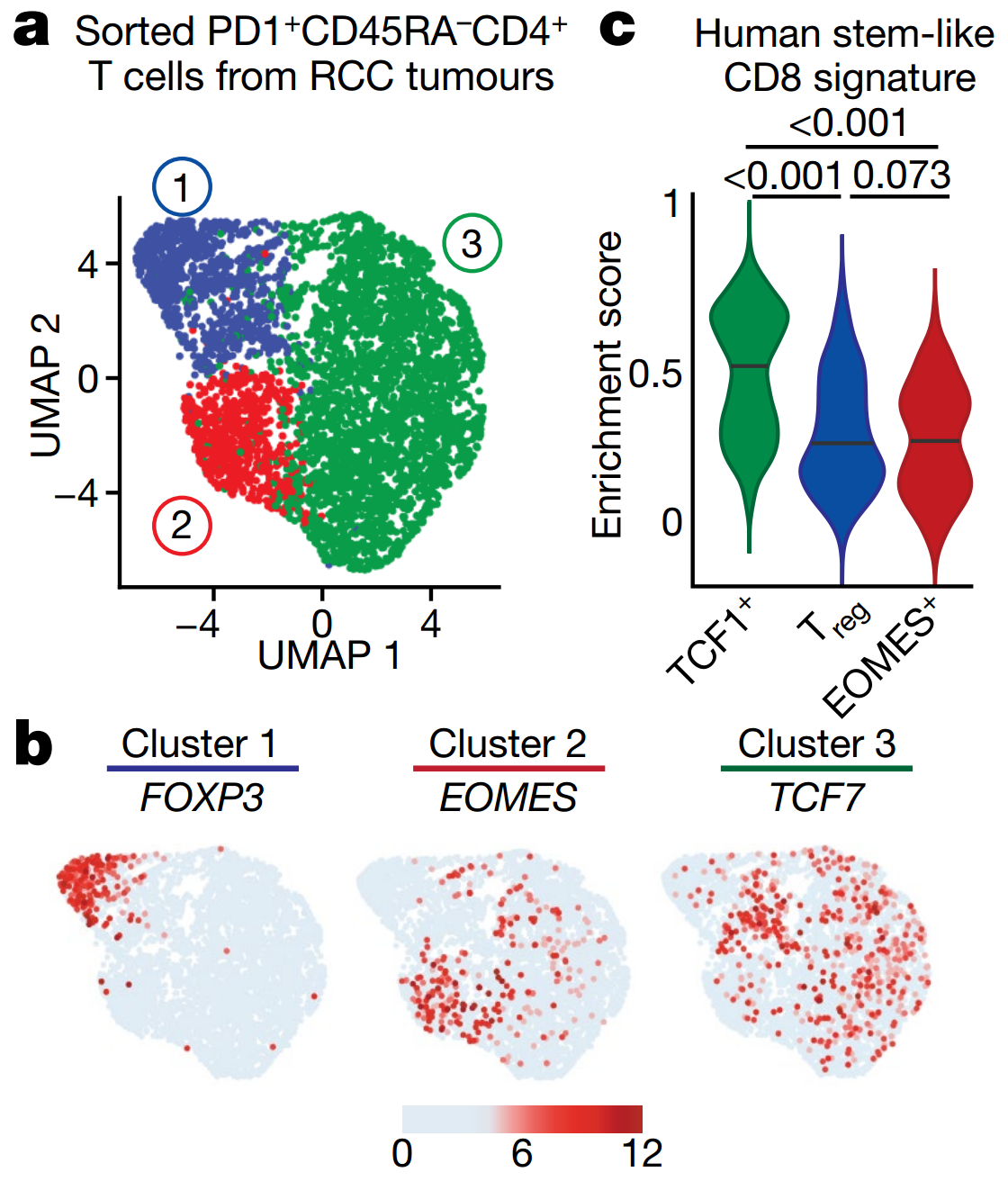
Understanding the diverse roles of CD4 T cells in cancer immunity has remained a challenge. A study conducted by researchers at the Winship Cancer Institute of Emory University offers critical insights. Using single-cell RNA sequencing (scRNA-seq) on CD4 T cells from kidney tumor environments, they identified three distinct clusters of these cells.
One cluster displayed a Treg phenotype, expressing markers such as FOXP3 and IL2RA, and exhibited suppressive characteristics.
Another cluster contained cytotoxic cells expressing EOMES and cytotoxic molecules but lacked a TH1 signature. The third cluster, however, was particularly intriguing. These cells lacked lineage-defining transcription factors like TBX21 or GATA3 and instead showed high expression of TCF7, a gene associated with stem-like properties.
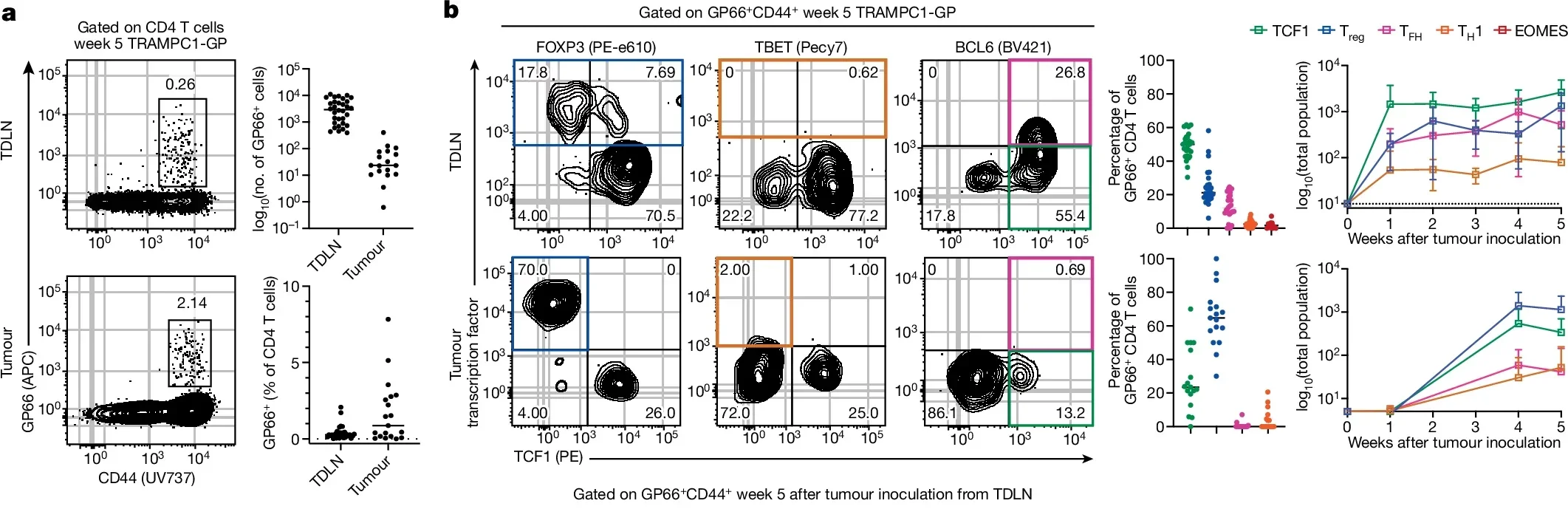
The stem-like CD4 T cell population, characterized by markers PD1 and TCF1, resides primarily in tumor-draining lymph nodes (TDLNs). These cells possess the ability to self-renew and differentiate into other immune cell types, making them a critical component of the immune system’s arsenal. However, their potential is often constrained by the suppressive influence of Tregs.
Related Stories
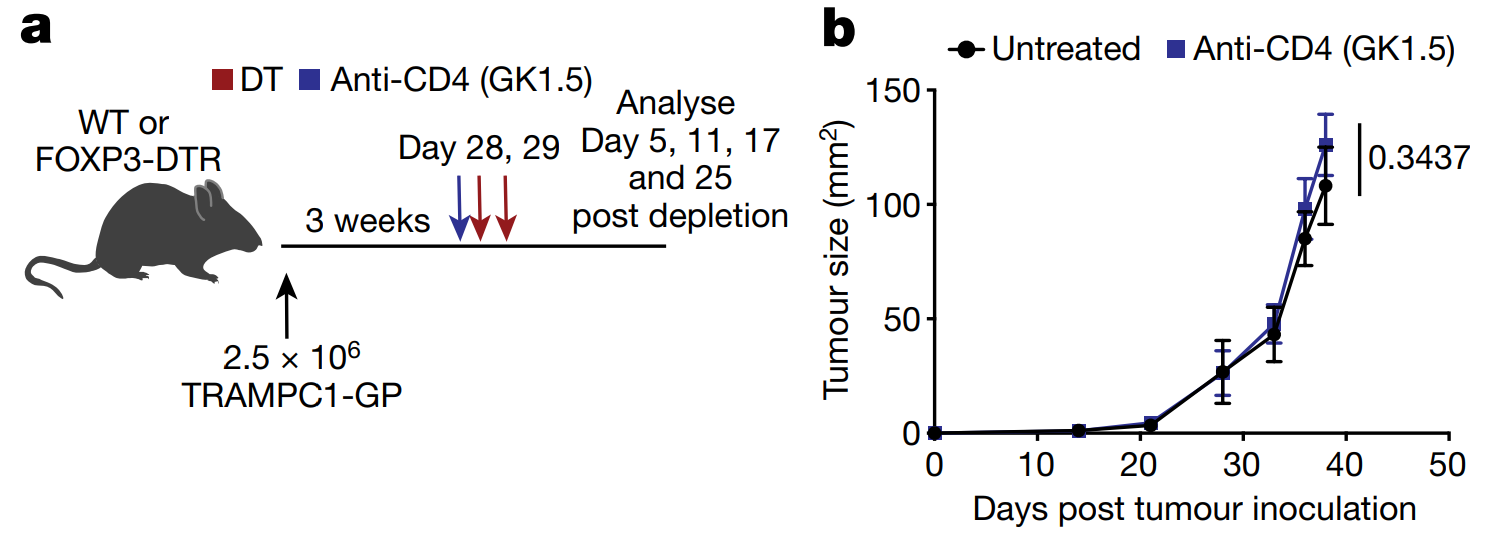
Researchers discovered that when Tregs were depleted, these stem-like CD4 T cells shifted from a quiescent state to an active one. This transition led to the production of TH1 cells, which enhanced the differentiation of CD8 T cells in TDLNs and triggered a powerful anti-tumor response.
“In around 10% of patients where the stem-like CD4 cell is active, there is a far more vigorous immune response to the cancer,” explains Haydn T. Kissick, PhD, a lead researcher on the study.
Notably, the presence of active TH1 cells in patients with kidney cancer was linked to successful immunotherapy outcomes and prolonged progression-free survival. This finding highlights the importance of these cells in determining the efficacy of cancer treatments.
While the potential of stem-like CD4 T cells is promising, their suppressive state in most patients presents a significant hurdle. This idle state prevents the immune system from effectively targeting tumors. First author Maria Cardenas emphasizes, “The stem-like CD4 T cell is capable of switching to an active state. It can restart a powerful anti-tumor immune response.”
To overcome this suppression, researchers are exploring ways to activate these cells and sustain their activity. Early experiments have shown that activating stem-like CD4 T cells can improve the effectiveness of PD1 blockade therapies, a common form of immunotherapy.
By enforcing the expression of the TBET transcription factor, scientists have successfully reprogrammed these cells to bypass their restricted state and induce robust immune responses.
Another promising approach involves using mRNA and lipid nanoparticle (LNP) technology to reprogram these cells. This method could effectively “teach” the stem-like CD4 T cells to remain active and mount continuous anti-tumor responses.
The discovery of stem-like CD4 T cells opens new avenues for cancer therapy. By understanding how these cells switch between active and suppressive states, researchers aim to develop strategies to improve immunotherapy outcomes for a broader range of patients.
The findings also emphasize the importance of the tumor microenvironment, particularly TDLNs, in shaping immune responses. Tregs in these areas play a pivotal role in maintaining the suppressive state of stem-like CD4 T cells. Targeting these regulatory mechanisms could unlock the full potential of the immune system in combating cancer.
Dr. Kissick notes the importance of collaboration and innovation in advancing this research: “Our Phase I Clinical Trials Unit is robust, and we have the contributions of physicians and patients here too. We have all the pieces of the puzzle; it’s just a matter of putting them together.”
The study, which involved a multidisciplinary team from the Winship Cancer Institute, highlights the collaborative effort required to address the challenges of cancer immunotherapy. Researchers such as Martin Sanda, MD, Mehmet Bilen, MD, and others contributed to the project, underscoring the need for expertise across various fields.
While the discovery of stem-like CD4 T cells is a significant step forward, many questions remain. Researchers need to better understand the mechanisms that regulate these cells and develop strategies to harness their potential effectively. Future studies will focus on translating these findings into clinical applications, with the hope of improving treatment outcomes for patients with cancer.
The promise of reprogramming stem-like CD4 T cells to fight tumors offers a new frontier in cancer immunotherapy. By leveraging advanced technologies and collaborative efforts, scientists are working to turn this promise into reality.
The journey is far from over, but each step brings us closer to unlocking the immune system’s full potential.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post Newly discovered immune cell revolutionizes cancer treatments appeared first on The Brighter Side of News.