The prevalence of substance use disorders, such as opioid and alcohol use disorders, has created a significant public health crisis. In the United States, drug overdose deaths surged from 18,000 in 1999 to over 107,000 in 2021. Alarmingly, opioids contributed to 75% of these fatalities.
Similarly, alcohol use disorder affects nearly 29.5 million people in the U.S., ranking as one of the leading causes of preventable deaths. Excessive alcohol consumption led to approximately 178,000 deaths annually between 2020 and 2021.
Amidst these alarming statistics, a novel avenue for addressing substance use disorders is emerging: repurposing medications typically used for diabetes and obesity management.
Recent findings from the journal Addiction highlight a promising link between glucagon-like peptide-1 receptor agonists (GLP-1 RAs), such as Ozempic, and reductions in substance-related behaviors. These medications were initially designed to treat Type 2 diabetes and obesity by regulating hunger and improving satiety.
GLP-1 RAs mimic the GLP-1 hormone, which interacts with receptors in the brain’s mesolimbic system—a region critical for processing rewards and motivated behaviors. This same brain region plays a significant role in the development and maintenance of addictive behaviors.
Because of the overlap between pathways governing food intake and substance use, researchers hypothesized that GLP-1 RAs could influence the “satiety” of addictive substances.
Animal studies have supported this hypothesis, showing that these drugs reduce alcohol intake and modify drug-seeking behaviors in rodents. Similarly, glucose-dependent insulinotropic polypeptide (GIP) agonists, such as Mounjaro, show potential for modulating reward pathways tied to addiction.
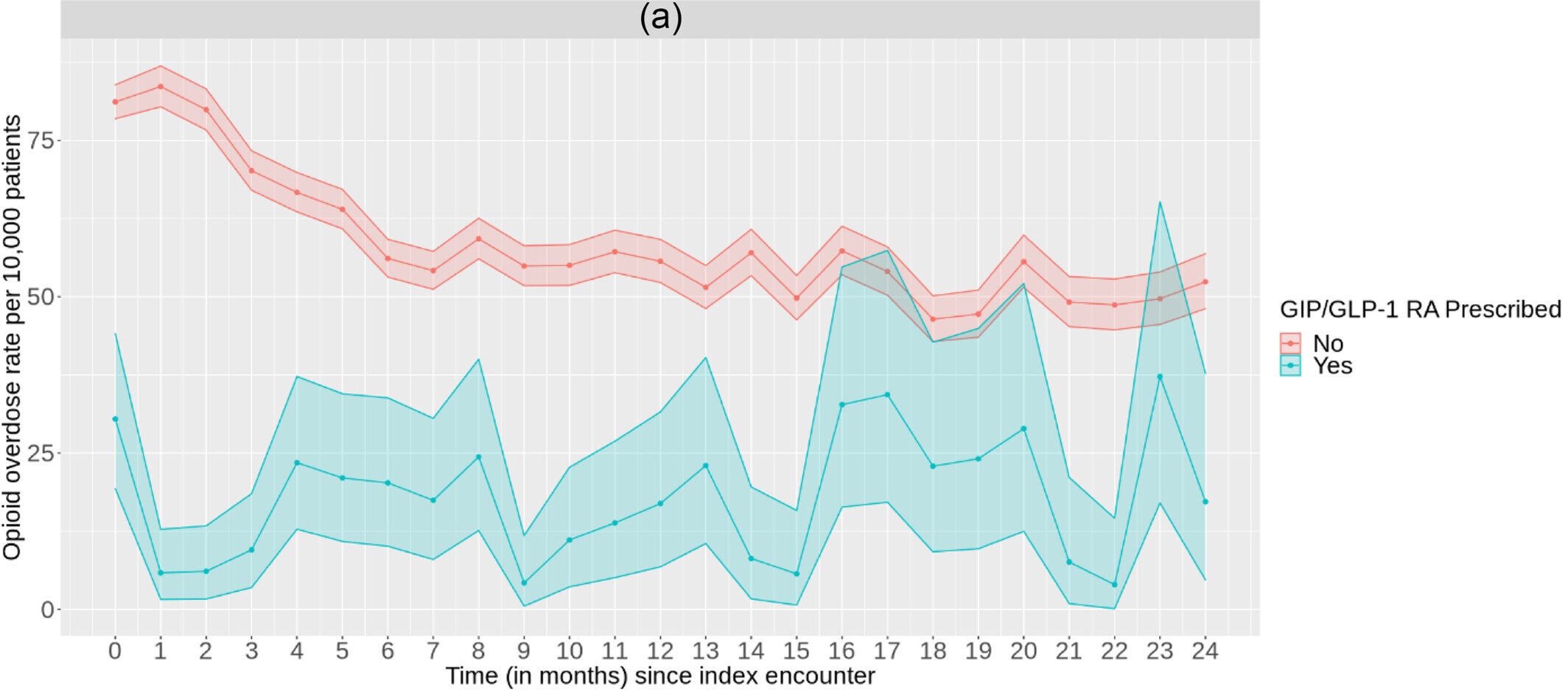
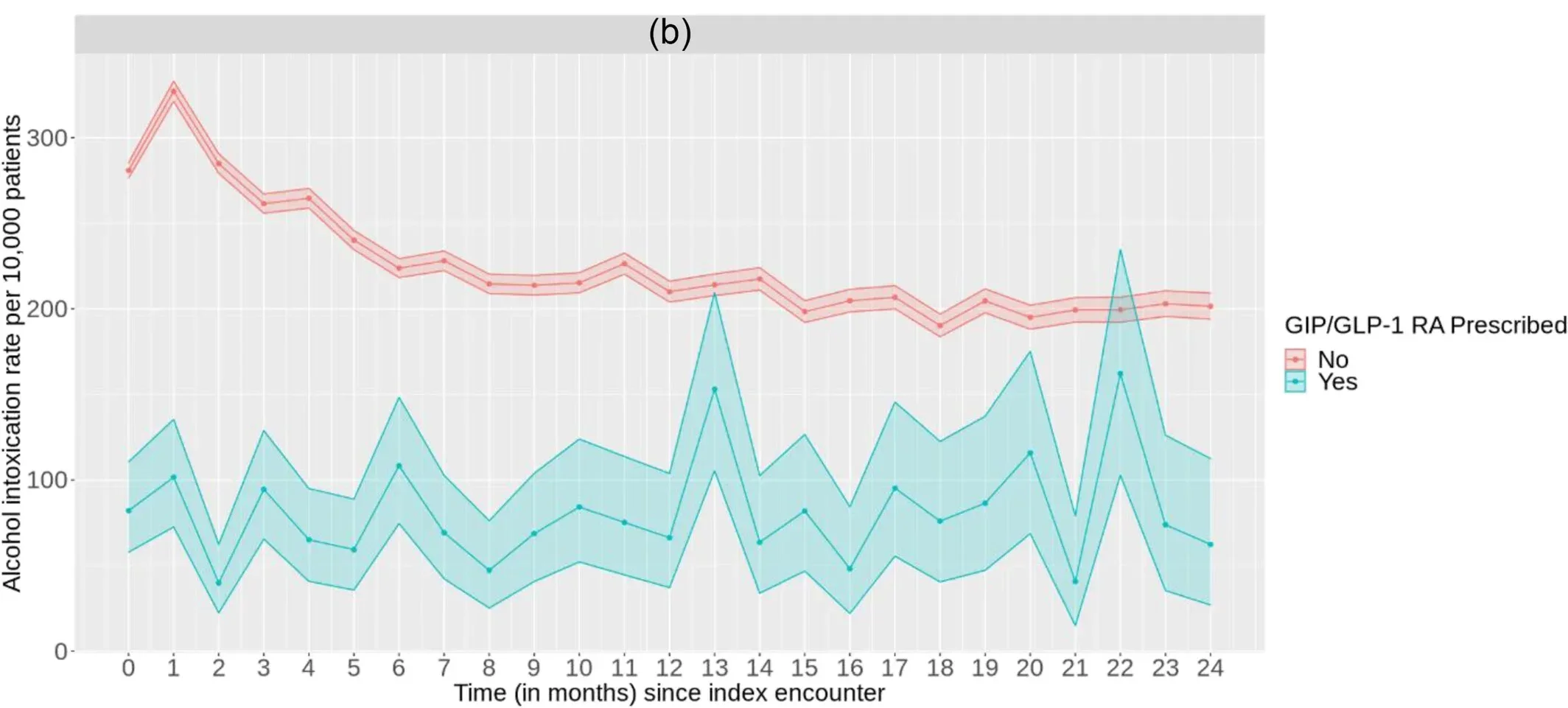
While animal studies and small-scale trials hinted at the potential of GLP-1 RAs and GIPs in addressing substance use disorders, a recent large-scale study provides the first robust evidence in human populations. Researchers analyzed data from over 1.3 million individuals with opioid use disorder (OUD) or alcohol use disorder (AUD), leveraging electronic health records to assess the impact of these medications.
Related Stories
The study examined 503,747 individuals with OUD, of whom 8,103 had prescriptions for GLP-1 RAs or GIPs. Results revealed that those prescribed these medications had a 40% lower rate of opioid overdose compared to their counterparts without prescriptions.
Similarly, the study assessed 817,309 individuals with AUD, including 5,621 prescribed GLP-1 RAs or GIPs. Among this group, rates of alcohol intoxication were 50% lower than those without these prescriptions.
The findings come at a critical time when barriers to conventional treatments for substance use disorders remain significant. Current evidence-based treatments, including medication-assisted therapy (MAT) for OUD and AUD, are underutilized due to stigma, limited access to prescribing providers, and socioeconomic challenges. Even when treatments are available, many patients continue to struggle with addiction, underscoring the need for alternative or complementary therapies.
GLP-1 RAs and GIPs offer a novel approach to addressing these gaps. By targeting overlapping pathways in addiction and metabolism, these drugs may complement existing pharmacological treatments. Moreover, their established safety profiles for diabetes and obesity management position them as attractive candidates for broader clinical applications.
Despite the promising results, further research is necessary to validate and expand upon these findings. Ongoing clinical trials are exploring the effects of GLP-1 RAs on substance-related outcomes such as cigarette smoking, opioid cravings, and alcohol consumption. However, these studies face limitations, including small sample sizes and a lack of generalizability to broader patient populations.
The recent large-scale study’s insights pave the way for more comprehensive investigations. Researchers aim to examine how GLP-1 RAs and GIPs impact individuals with comorbid conditions like Type 2 diabetes and obesity, which often coexist with substance use disorders.
Understanding these relationships could revolutionize treatment strategies for addiction, offering hope for millions affected by these chronic conditions.
As public health crises related to opioids and alcohol continue to escalate, innovative solutions are crucial. Medications like Ozempic and Mounjaro may hold the key to not only improving metabolic health but also addressing the neurobiological underpinnings of addiction.
By bridging the gap between metabolic and addiction research, these drugs could redefine the landscape of substance use disorder treatment, providing a lifeline to those in need.
Note: Materials provided above by The Brighter Side of News. Content may be edited for style and length.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post Ozempic: A new hope for opioid and alcohol addiction treatment appeared first on The Brighter Side of News.