Injections are rarely enjoyable, but frequent doses can become particularly burdensome. Scientists have now developed a new drug delivery system that uses tiny crystals to significantly reduce how often you’ll need injections. By creating a “drug depot” under the skin, these crystals slowly release medication, potentially lasting months or even years with just one shot.
Researchers from MIT have designed this crystal-based injectable method to overcome some major limitations of current treatments. Traditional injections, especially those required for contraception or chronic illnesses, must be repeated often.
Current long-term injections available in clinics usually last only about three months and often involve large, uncomfortable needles. The new method, however, allows for easy injections through smaller needles while providing stable and prolonged drug release.
This innovation began with a clear goal: creating an easy-to-use, long-lasting contraceptive option for women, particularly in developing countries. As lead researcher Vivian Feig explains, “The overarching goal is to give women access to a lot of different formats for contraception that are easy to administer, compatible with being used in the developing world, and have a range of different timeframes of durations of action.”
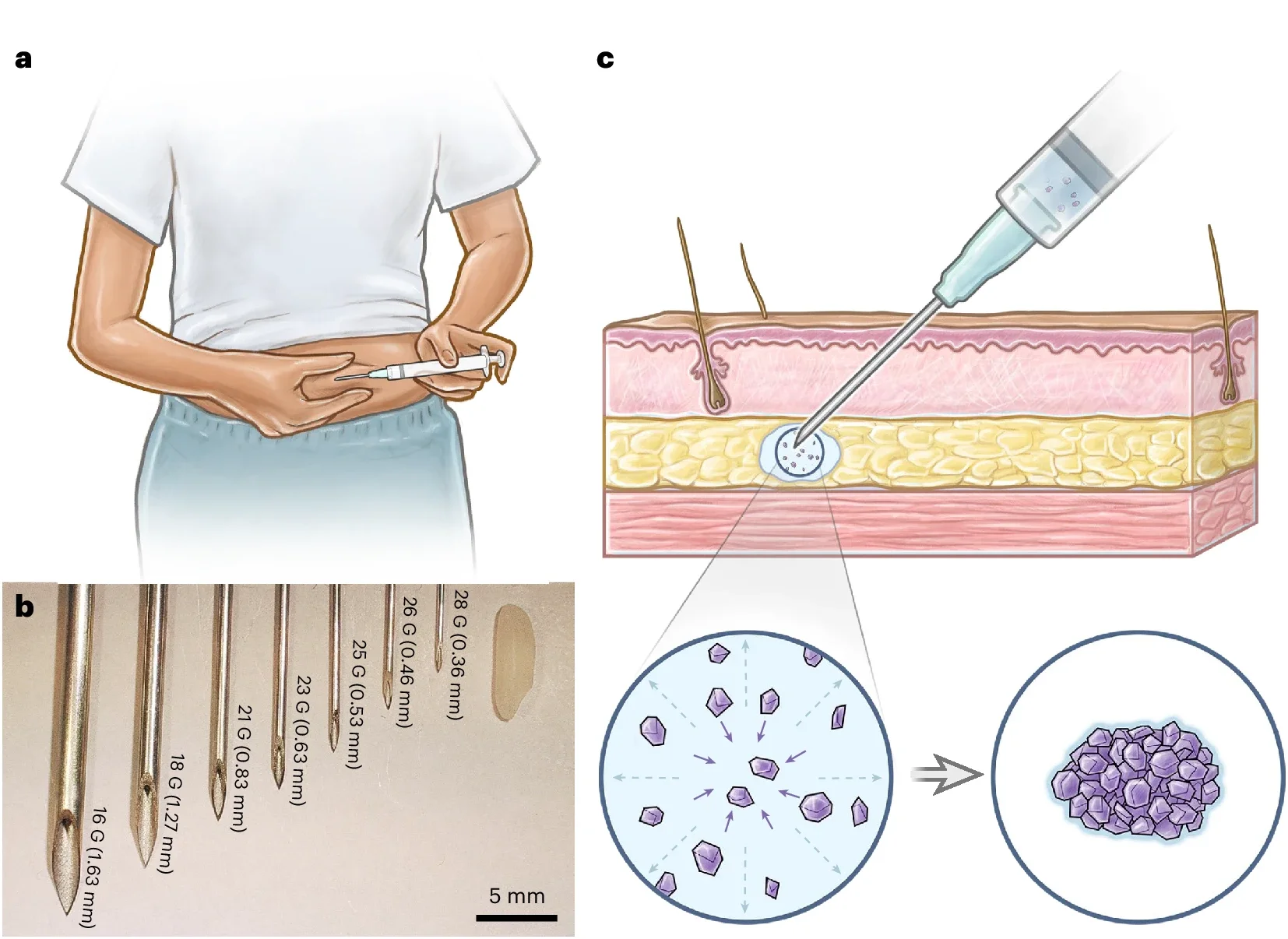
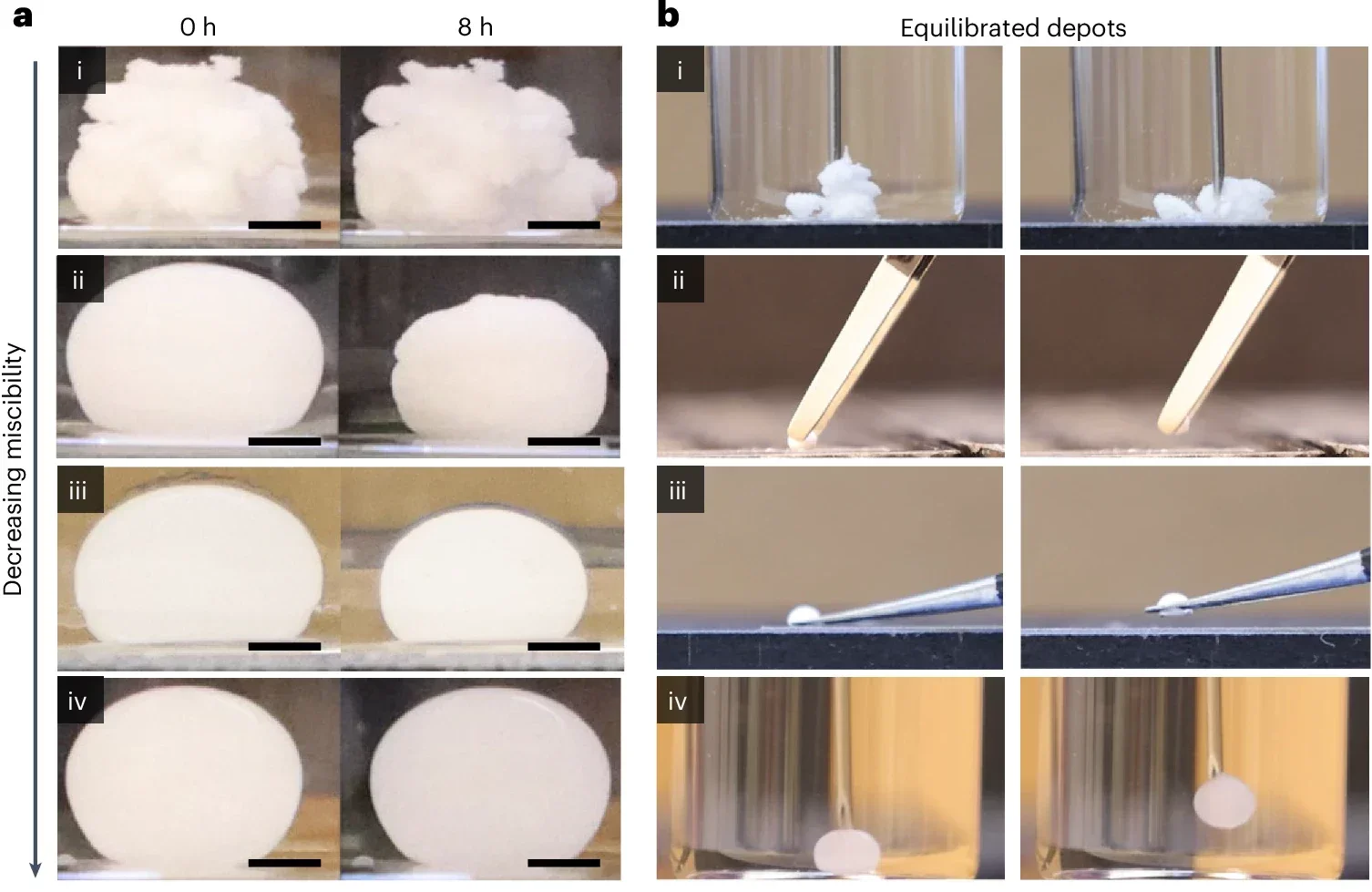
The researchers focused on a contraceptive hormone called levonorgestrel, known for its ability to crystallize. When mixed with a special solvent called benzyl benzoate, these crystals stay fluid enough to pass through very thin needles. After injection under your skin, the crystals self-assemble into a compact, solid drug depot.
According to Giovanni Traverso, senior author of the study, “The solvent is critical because it allows you to inject the fluid through a small needle, but once in place, the crystals self-assemble into a drug depot.” This depot structure reduces the drug’s surface area, slowing down its release. The system avoids heavy use of polymers typically found in similar treatments, keeping injections simple and patient-friendly.
Related Stories
While polymers usually make long-lasting injections difficult by thickening solutions, the MIT researchers cleverly bypassed this issue. They used a very small amount of biodegradable polymer—less than 1.6 percent by weight—to help control the speed of drug release without sacrificing ease of injection.
Graduate student Sanghyun Park explains, “By incorporating a very small amount of polymers—less than 1.6 percent by weight—we can modulate the drug release rate, extending its duration while maintaining injectability. This demonstrates the tunability of our system, which can be engineered to accommodate a broader range of contraceptive needs as well as tailored dosing regimens for other therapeutic applications.”
This minimal polymer addition makes the system highly flexible. Doctors and pharmacists could adapt the crystal depot system for other drugs, ranging from contraceptives to treatments for HIV, tuberculosis, or mental health conditions. The possibilities for tailored medication dosage and scheduling are extensive.
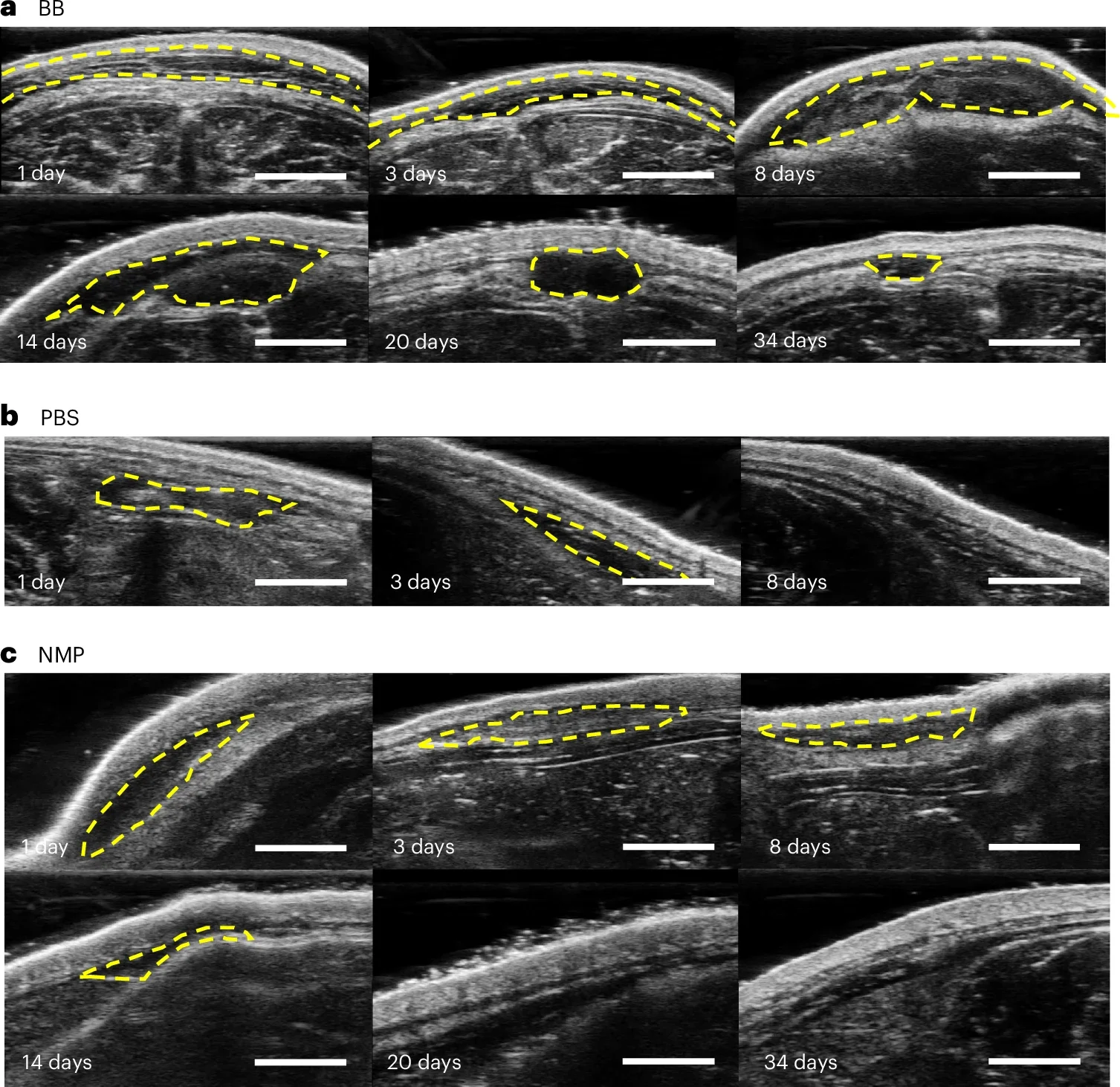
Early tests with rats provided strong evidence that this depot can sustain steady drug release. Three months after a single injection, the depot remained mostly intact, with 85 percent of the medication still unreleased. Researchers believe that these depots could continue to provide medication for well over a year.
“We anticipate that the depots could last for more than a year, based on our post-analysis of preclinical data. Follow-up studies are underway to further validate their efficacy beyond this initial proof-of-concept,” Park said.
Importantly, unlike many injectable systems currently in use, these crystal depots can be removed easily if your treatment needs change. Once formed, the depot remains compact enough for a doctor to remove it surgically if necessary. This capability adds a critical safety and flexibility benefit, particularly useful for contraceptive treatments where reversing the medication effect might be needed to restore fertility.
Currently, long-lasting injectables fall into two main categories: microparticle suspensions and implants formed inside your body. Both methods have limitations, often requiring thick solutions that force doctors to use large needles, making the injections uncomfortable and difficult to self-administer. Because the crystal-based method relies less on polymers, it can pass through much thinner needles, greatly improving patient comfort.
Smaller needles also mean fewer side effects such as bruising or bleeding. As studies show, patients prefer smaller needles, leading to greater acceptance and potentially better adherence to medication plans. This feature is especially critical in developing regions, where medical visits are harder to schedule regularly.
The need for reliable, long-acting contraception is particularly urgent in low-resource areas. Currently, injectable contraceptives available for self-administration last only around three months, requiring frequent injections. The MIT crystal depot method could extend this duration dramatically, possibly matching surgically placed implants like Nexplanon, which lasts over a year.
“Now we’re considering which indications we go after: Is it contraception? Is it others? These are some of the things that we’re starting to look into as part of the next steps toward translation to humans,” Traverso adds. The simple, low-cost nature of the crystal injection system could significantly boost access to critical medications, improving health outcomes globally.
While initial results are promising, researchers recognize the journey from laboratory success to widespread clinical use is lengthy. The next stages involve thorough safety tests, ensuring this crystal depot system behaves consistently in humans.
Traverso’s team is already planning advanced preclinical studies. These will explore exactly how the crystals form their stable depot structures under conditions closer to human skin. Moving forward, the crystal depot technology will be evaluated for safety, reliability, and effectiveness across various drugs.
Ultimately, this crystal injection method could transform how chronic illnesses, contraception, and diseases requiring steady medication intake are managed. The long-term impact on patient care and comfort could be substantial, particularly for millions who currently struggle with frequent injections or limited healthcare access.
Research findings are published in the journal Nature Chemical Engineering.
Note: The article above provided above by The Brighter Side of News.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post Tiny crystals offer long-lasting drug delivery without the pain appeared first on The Brighter Side of News.
Leave a comment
You must be logged in to post a comment.