Low back pain is one of those problems that can sneak into daily life and refuse to leave. It can make it harder to work, sleep, or even sit through a meal. Doctors have long known that many factors raise the risk, including stress, poor sleep, aging, smoking, and inactivity. Weight has often been discussed too, but past studies were usually small or focused on narrow groups. Now, a large new study from Boston University’s Chobanian & Avedisian School of Medicine brings clearer answers.
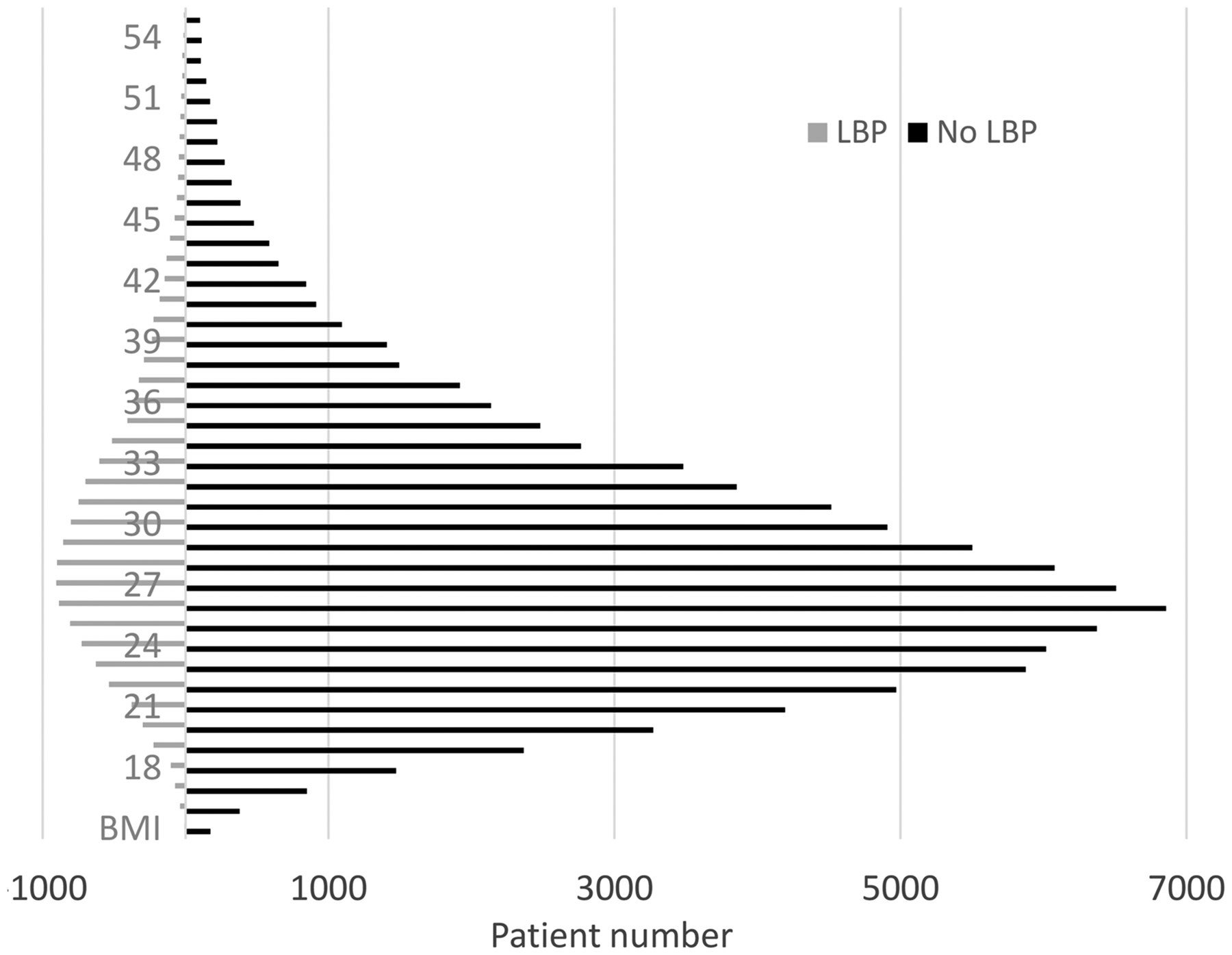
The research shows that adults who are overweight or obese face a much higher chance of developing low back pain than those in a healthy weight range. The team reviewed medical records from more than 110,000 adults who visited an urban teaching hospital for outpatient care over one year. The size of this group makes the results hard to ignore.
Michael D. Perloff, MD, PhD, an assistant professor of neurology at the school and the study’s corresponding author, says the findings fit what many clinicians see every day. “Low back pain is one of the most common complaints patients have for their medical providers. While medications, formal physical therapy and other treatments can help, correcting risk factors, such as smoking or deconditioning, also help LBP. The current study suggests weight control and maintaining a lower BMI in the healthy range, can be beneficial for LBP symptoms as well.”
Low back pain does not only hurt. It also disrupts work, family life, and mood. It remains a leading cause of disability and work loss, and it carries a large cost for health systems. When pain lingers, people often need repeat visits, imaging tests, medications, and physical therapy. Some even face surgery.
You might already know that stress or poor sleep can make pain worse. You might also know that staying active can help protect the back. What has been less clear is how much body weight alone changes the risk in everyday medical settings.
Earlier studies tried to answer this, but many had limits. Some included fewer than 1,000 patients. Others focused on special groups, such as young men or people already in pain clinics. Those results did not always reflect the general population. The new study fills that gap by looking at a very large and mixed group of adults.
The research team used computer analysis to review electronic medical records from more than 110,000 adults aged 18 or older. All had visited the same urban teaching hospital for outpatient care during a single year.
For each patient, the records included age, sex at birth, height, weight, and body mass index, also called BMI. The team also noted whether low back pain appeared as a complaint during the visit.
BMI is a simple number based on height and weight. A BMI around 18 to 24.9 usually falls in the healthy range. A BMI from 25 to 29.9 counts as overweight. A BMI of 30 or higher counts as obese.
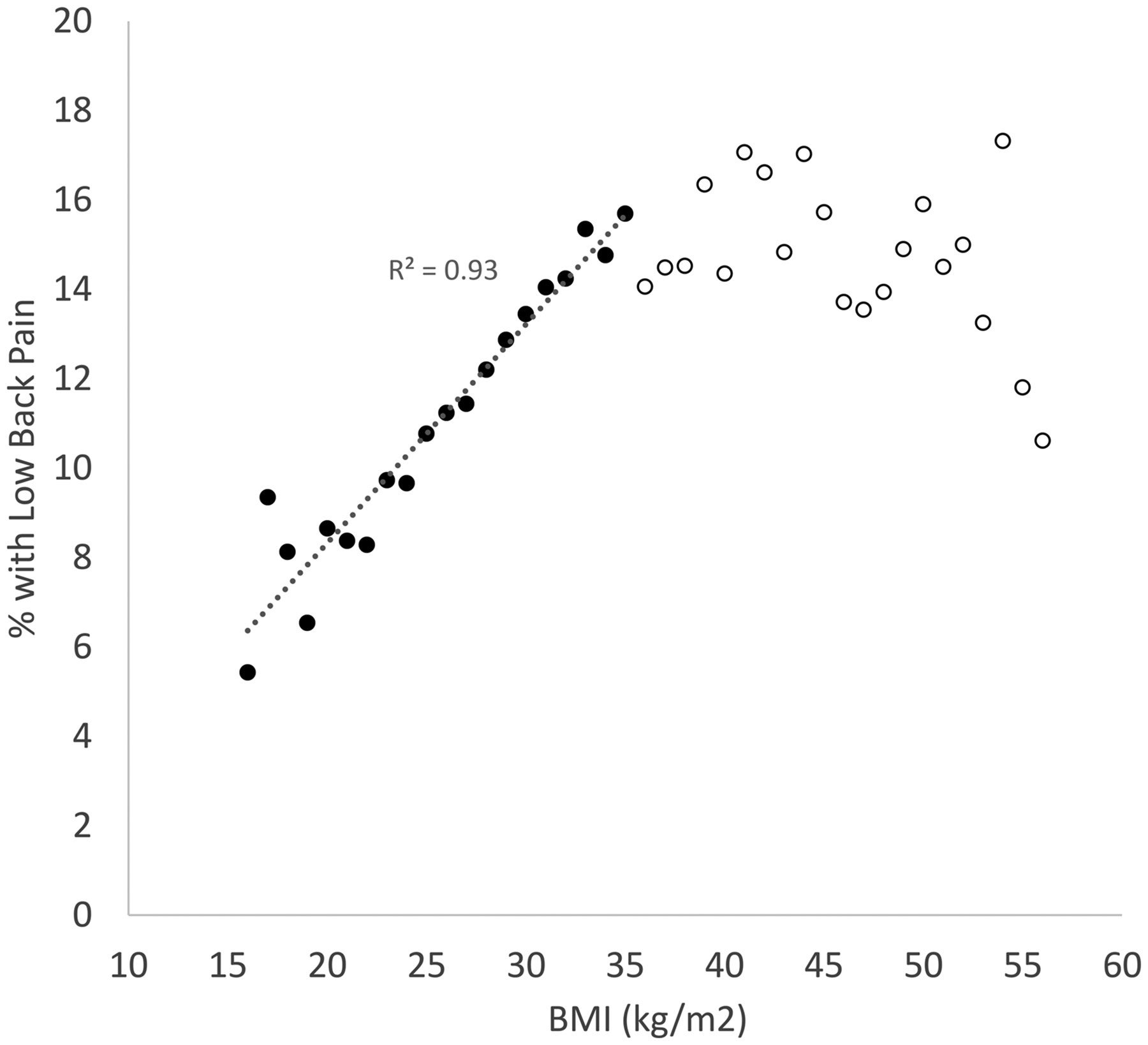
The researchers then looked for patterns between BMI and how often patients reported low back pain.
“Our results showed a strong and steady rise in back pain reports as BMI increased from 18 up to 35. In simple terms, as weight went up within this range, so did the chance of having low back pain,” Perloff told The Brighter Side of News.
“The numbers help explain the trend. For every one-unit increase in BMI between 18 and 35, the prevalence of low back pain rose by about 7 percent. The study also described this as roughly a 10-pound increase in weight for many adults,” he continued.
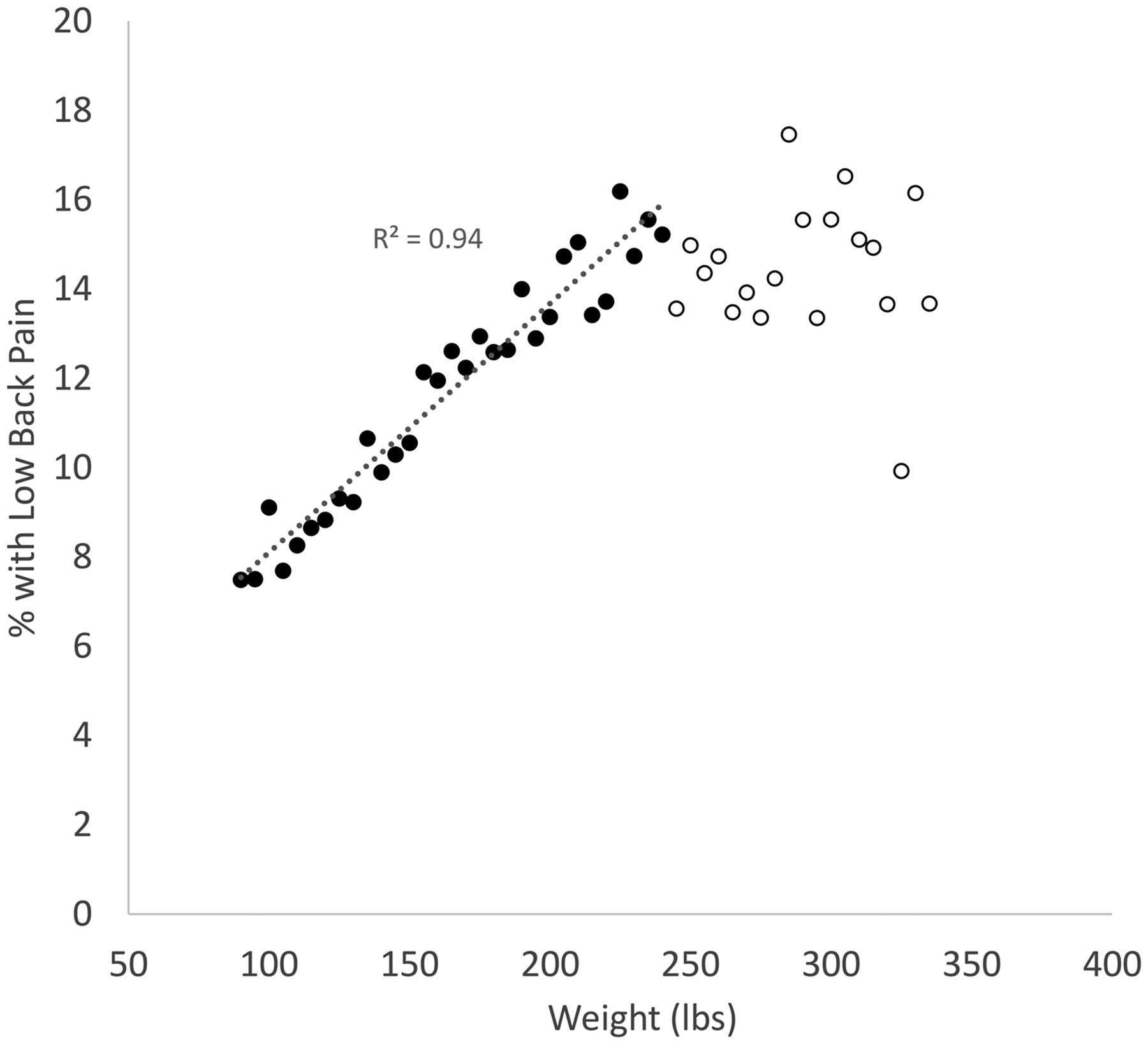
That means a person with a BMI of 30 had a much higher chance of reporting back pain than someone with a BMI of 25. And someone at 35 faced even more risk than both.
Interestingly, once BMI went above 35, the rise stopped. The rate of back pain did not keep increasing. It stayed at about the same level. The study did not explain why this leveling happened, but it clearly showed that the risk climbs steeply before that point.
Not everyone with a higher BMI will develop back pain. Some people at higher weights never report it. Still, the pattern across more than 110,000 patients shows that risk grows as weight grows.
For doctors, this helps explain why back pain appears so often alongside weight gain. For patients, it offers another reason to take weight seriously as part of overall health, not only for the heart or joints, but also for the spine.
Perloff, who also directs pain medicine at Boston Medical Center, says the message is not about blame. It is about risk. “Our study strongly suggest that maintaining a healthy weight or BMI is likely helpful at avoiding low back pain,” he said.

The study did not test causes, but several ideas help explain the link.
Extra weight can place more stress on the spine and the muscles that support it. Over time, that added load may strain discs, joints, and ligaments. Posture can also change with weight gain, which may shift how force moves through the lower back.
Weight may also link to lower activity levels. When movement drops, muscles that protect the spine can weaken. That can make injury or pain more likely.
There may also be metabolic or inflammatory effects tied to higher body fat that influence pain, though this study did not examine those factors.
What makes this research different is its scale and setting. More than 110,000 patients provide a picture that is closer to everyday clinical life. The data came from routine outpatient visits, not from a special pain clinic or a narrow group.
Because of that, the findings apply more broadly to adults who seek medical care in cities and similar settings. The study also avoided a common problem in earlier research, which is drawing strong conclusions from small or selective samples.
Still, the authors note important limits. The study shows a link, not proof of cause. It also does not describe how long pain lasted, how severe it was, or how it affected daily function. It only records whether back pain was reported during the visit.
Future studies could follow people over time to see whether weight changes lead to changes in back pain risk. Others could test whether weight loss programs reduce new cases of low back pain or make existing pain easier to manage.
Researchers may also look at how exercise, muscle strength, and flexibility interact with BMI to shape risk. The current findings give those studies a strong reason to move forward.
These findings suggest that weight management should stand alongside other well-known steps to protect the back, such as staying active, avoiding smoking, and addressing stress and sleep problems.
For patients, this means that keeping BMI in a healthy range may lower the chance of developing low back pain or reduce how often it appears. For those who already have pain, weight control may support other treatments like physical therapy or exercise.
For clinicians, the results support talking about weight in a practical and supportive way when treating back pain. It becomes part of a broader plan that looks at the whole person, not only the painful area.
For health systems, prevention efforts that help people maintain healthy weight could reduce the long-term burden of back pain, including lost work days and repeated treatments.
Over time, this approach could save costs and improve quality of life for many people.
Research findings are available online in the journal Pain Medicine.
Like these kind of feel good stories? Get The Brighter Side of News’ newsletter.
The post Why weight matters more than you think for your lower back appeared first on The Brighter Side of News.